Parotid Node Metastases in Locally Advanced Nasopharyngeal and Oropharyngeal Cancer
To determine the frequency and clinical characteristics of parotid gland metastasis from nasopharyngeal cancer and oropharyngeal cancer and define criteria for elective inclusion of parotidean nodes in the radiotherapy clinical target volume.
Abstract
Purpose:To determine the frequency and clinical characteristics of parotid gland metastasis (PGM) from nasopharyngeal cancer (NPC) and oropharyngeal cancer (OPC) and define criteria for elective inclusion of parotidean nodes in the radiotherapy clinical target volume (CTV).
Methods and Materials:All cases of NPC and stage III/IV OPC referred for radiotherapy at our institution between 2003 and 2011 were reviewed. Incidence and risk factors for PGM at presentation and at time of failure were analyzed. A literature review of PGM incidence in head and neck squamous cell carcinoma was performed.
Results:Of 52 NPC and 231 OPC patients, two (3.8%) NPC patients and 4 (1.9%) patients presented with PGM. All PGMs were located ipsilateral to the primary tumors in patients with bulky, ipsilateral level II and multi-level ipsilateral lymph node involvement of aggregate size greater than 6 cm in diameter. Similar rates and characteristics were found in the literature after an extensive search.
Conclusion:The ipsilateral parotidean nodes may be at risk of metastatic involvement when bulky ipsilateral level II metastases and multi-level nodal disease are co-existent, possibly due to retrograde lymphatic drainage. Inclusion of the ipsilateral parotid gland in the CTV should be considered in such cases.
Introduction
The most common oral complication and cause for reductions of quality of life (QOL) after head and neck radiation is salivary gland dysfunction and xerostomia.1,2Parotid gland-sparing intensity-modulated radiation therapy (IMRT) techniques have become standard of care in an attempt to prevent salivary flow dysfunction and xerostomia. IMRT has facilitated parotid-sparing by virtue of enabling steep dose gradients between normal tissue and clinical target volumes (CTV) in close apposition. Indeed, the use of IMRT has increased dramatically in the United States.3Furthermore, in comparisons between IMRT and conventional radiation for head and neck cancer (HNC), no significant increases in the rate of locoregional relapse have been found with the use of IMRT.4-6Given the steep dose gradients typical of IMRT, awareness of the risk of involvement to various adjacent sites is critical for appropriate target delineation and avoidance of marginal failures.
While the presence of clinically-evident disease in a parotid gland (PG) precludes its exclusion from the radiation target volume, there has been some controversy as to whether the ipsilateral PG should be spared when it is not clinically involved.4,7Although the PG should likely be included in the CTV when it is at high risk for sub-clinical disease, no clear clinical factors to-date have been identified to indicate when the PG is at high risk. Others have previously reported recurrences in the region of a spared PG after IMRT.4,5In a publication by Chao et al, a patient with squamous cell carcinoma (SCC) of the piriform sinus developed a surgical bed recurrence near the spared PG.5Cannon et al, also reported 3 additional cases of tumor recurrence in the region of the spared PG.4Two of these recurrences were in peri-parotid lymph nodes (LNs), and the third in the skin near the tail of the spared PG. An additional 3 cases of peri-parotid metastases have been reported by Chen et al,8with all 3 recurrences occurring in or near the spared contralateral PG. However, the overall frequency of these recurrences has not been well-reported.
In the present study, we sought to identify cases of pathologically-proven PG metastases in patients with previously-untreated nasopharyngeal and oropharyngeal cancer (NPC and OPC, respectively), perform a review of the relevant literature on PG metastases in head and neck squamous cell carcinoma (HNSCC), and determine common clinical characteristics of patients with PGM to generate indications for inclusion of the PG in the CTV.
Methods and Materials
This retrospective study was approved by the University of Michigan IRB. Existing databases of all cases of NPC and Stage III/IV OPC presenting for consultation at the Department of Radiation Oncology from 2003-2011 were queried to identify patients with clinical and/or radiological evidence of PG metastases. Cases of SCC metastatic to the parotid when the primary site was unknown were excluded. The presence of metastases within the parotid gland, rather than within level II, was confirmed in all cases by an attending neuroradiologist. Clinical characteristics of patients with confirmed PGM were retrospectively reviewed. A PubMed literature review was performed to determine the incidence of parotid metastasis (PM) from mucosal HNC, and potentially identify clinical factors predisposing patients to metastatic dissemination to the PG.
Results
Between 2003 and 2011, 52 patients with NPC and 231 patients with OPC were identified. Of these, 2 of 52 (3.8%) patients with NPC and 4 of 231 (1.7%) with OPC presented with PMs. All PGM were ipsilateral to the primary tumor, and all patients had extensive multilevel ipsilateral nodal involvement with bulky level II adenopathy. Of all nasopharynx and oropharynx cases that presented to us from 2003 to 2011, 33 patients had N3 disease.
Three of the 6 patients with PGM underwent definitive chemoradiation using IMRT at our institution. Of these 3, no LRR has been observed thus far, at a median follow-up of 14 months (range 9-21). In addition, no patient who presented to us with oral cavity, larynx, or hypopharynx primary carcinomas presented with PG involvement. The clinical details of the 6 patients presenting with PGM are discussed below.
Case 1
A 52 year old man with Stage III T2N2M0 nasopharyngeal carcinoma presented with lateral retropharyngeal lymphadenopathy, junctional lymphadenopathy, as well as extensive LN involvement ipsilaterally in levels II-IV, including upper level II. In addition, he was found to have an enlarged LN in the PG tail, and additional suspicious peri-parotid LNs more inferiorly. Fine needle aspiration was performed on the enlarged parotidean node and returned positive for nasopharyngeal carcinoma. This patient elected to pursue chemoradiation outside of our institution and was subsequently lost to follow-up.
Case 2
A 21 year old female with Stage IVA T4N1M0 nasopharynx carcinoma presented to our institution with a large right, infiltrative nasopharynx primary tumor. CT and MR imaging revealed multiple, bulky upper ipsilateral level II nodes, as well as a biopsy-confirmed large right intraparotid lymph node. She was treated with definitive concurrent chemoradiation with IMRT at our institution, with all gross disease receiving 70 Gy in 35 fractions, followed by 2 cycles of adjuvant cisplatin and 5-fluorouracil. Six months after radiation, she developed osseous metastases and was treated with palliative radiation, though remained without evidence of local-regional recurrence (LRR) at 21 months after chemoradiation.
Case 3
A 54 year old male with a Stage IVA T3N2cM0 left tonsillar SCC presented with associated large, necrotic ipsilateral LNs in level II. In addition, a large necrotic LN mass was noted in the inferior tail of the parotid. Fine needle aspiration was performed on this enlarged node and returned positive. The presence of the PM occurred in the absence of nasopharyngeal extension of the primary mass. He received definitive concurrent chemoradiation, and the PG and necrotic LN mass were included in the treatment volumes, with the gross disease receiving 70 Gy in 35 fractions. He remained without evidence of recurrence at 9 months after chemoradiation.
Case 4
A 56 year old male, heavy smoker, with Stage IVB T3N3M0 HPV-negative invasive SCC of the left tonsil presented with diffuse lymphadenopathy, particularly with advanced, bulky level IB and II ipsilateral disease. The PET-CT revealed a left parotidean LN which was fluorodeoxyglucose (FDG)-avid, and biopsied positive. The patient elected to pursue definitive concurrent chemoradiation outside our institution.
Case 5
A 49 year old male with Stage IVA T2N2cM0 HPV-positive poorly differentiated SCC of the base of tongue initially presented with multi-level lymphadenopathy with diffuse involvement of level I and levels IIIII bilaterally, as well as a large necrotic LN mass in the left PG. An ipsilateral level I-IV selective neck dissection was performed, and the enlarged LN was found at the inferior portion of the lateral PG. All LN levels and the inferior parotid mass were positive for SCC. He received post-operative concurrent chemoradiation, with all gross tumor receiving 70 Gy in 35 fractions. He developed lung metastases 9 months after treatment completion, but has no evidence of LRR 14 months after treatment.
Case 6
Literature Search
A 57 year old male with Stage IVA T1N2cM0 HPVpositive SCC of the glossotonsillar sulcus presented with massive ipsilateral lymphadenopathy (levels II, III, and V), right carotid artery encasement, and left cervical lymphadenopathy (levels II and III). In addition, an FDG-avid lesion in the inferior portion of the right PG was noted. Fine needle aspirate (FNA) of the parotid lesion returned positive. He was referred for definitive concurrent chemoradiation outside our institution.
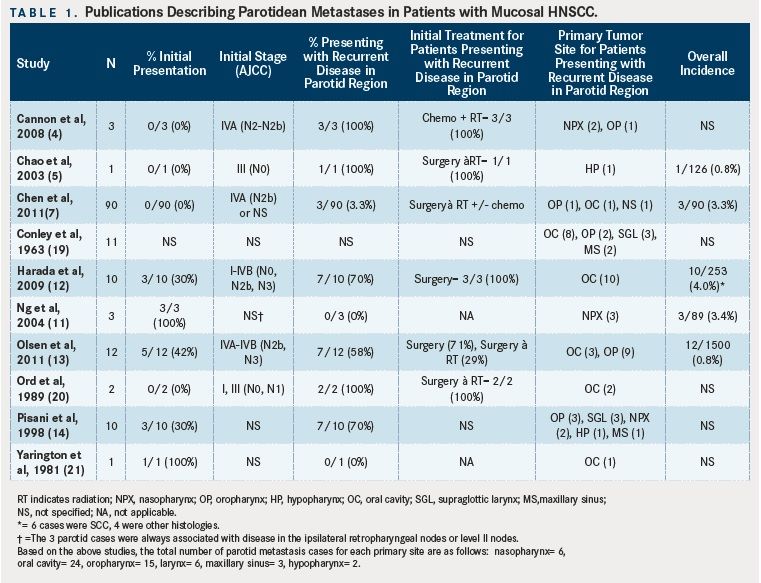
TABLE 1
The results of a literature search for patients with mucosal HNC who developed PG metastases, either at initial presentation or at recurrence are shown in. Many series do not report the overall incidence of PG metastases in mucosal HNSCC. Of those that do, the incidence of PMs appears to be 4% or less, consistent with the findings in the present series.
Discussion
Based on anatomic/radiologic studies, lymphatic drainage from the PG generally follows an orderly fashion, from intraparotid and periparotid LNs, to ipsilateral level II and III LNs. While both PM at initial presentation and recurrences in the parotid bed after therapy are rare, it is clear that the extensive network of intraparotid lymphatics puts the parotid region at risk for dissemination of tumor cells from a wide variety of HNC sites. As locoregional control improves with more modern therapy, identifying factors which predispose mucosal HNC patients to developing PMs bears significant importance for radiation. In patients receiving IMRT, Cannon and Lee documented 3 cases of patients with peri-or intra-parotid recurrences who had no evidence of parotid involvement on pre-treatment imaging. In their report and associated editorials, it has been postulated that altered lymphatic anatomy in the cervical lymphatics after surgery or definitive chemoradiation could contribute to these LRRs, in addition to natural routes of lymphatic dissemination that exist.4, 9, 10
In nasopharyngeal cancer, level II and retropharyngeal LNs represent the primary route of lymphatic drainage. Fletcher and Million documented that the incidence of peri-parotid/parotid/pre-auricular LN involvement at presentation for nasopharyngeal cancer is about 1% to 2%. Furthermore, radiologic studies combining MRI and FDG-PET have demonstrated an incidence of 3.4% of parotid bed nodal metastases in patients with nasopharyngeal carcinoma.11 These rates of parotid LN involvement in nasopharyngeal carcinoma are consistent with our institutional experience. Parotid LN involvement can potentially be attributed to known pathways of spread through lymphatic channels directly draining the Eustachian tube in the region of the nasopharyngeal tumor, which were originally depicted by Rouviere. However, as the Eustachian tube is frequently involved in advanced nasopharyngeal cancer, if this route was responsible for PM, it is likely that we would have observed these metastases with higher frequency than we have in our (and other) series.
In the literature, involvement of the PG from oral cavity and oropharynx primaries appears to be very infrequent. In a large surgical series of 1500 patients, Olsen et al, reported an overall incidence ~1% with oral cavity/oropharynx primary SCCs with pathologically-proven PG involvement. While 42% of these cases were associated with disease at presentation, 58% resulted from recurrences after the primary disease was treated. The majority of these metastases occurred in the inferior portion (tail) of the PG. Another surgical series reported on 239 patients with oral cavity SCC who underwent elective parotid tail resection (below the marginal mandibular branch of the facial nerve).12Parotid node involvement occurred in 2.5% of the cases. Furthermore, they observed an increased risk of parotid node involvement with an increased number of involved cervical nodes. There were 14.3% of patients with 3 or more LNs had PMs, compared to less than 2% with only 1-2 positive cervical LNs. In this report, we document 4 of 231 (1.7%) cases of oropharyngeal cancer with biopsy-proven involvement of the PG at initial presentation, consistent with that reported in the literature. To our knowledge, there is no evidence citing direct drainage from oropharyngeal tumors to the PG. In addition, our cases argue against the notion that all PMs result from direct spread from the mucosa to parotidean LNs.
Diffuse and bulky involvement of the ipsilateral upper jugular chain (especially upper level II) was common among all 6 of our observed cases of biopsy- proven PG metastases. In fact, all 6 cases had advanced ipsilateral nodal disease with an aggregate lymph node mass having a total largest dimension > 6 cm. We believe that this commonality is the driving force for PG involvement, and is likely due to retrograde flow from heavily obstructed, tumorladen level II-III ipsilateral lymphatics. This was also observed by Ng et al in their MRI and fluorodeoxyglucose FDG-PET imaging-based survey of nasopharyngeal carcinoma: all 3 patients who presented with PG metastases had significant disease either in the ipsilateral retropharyngeal or level II LNs.11Furthermore, all 5 patients in the report by Olsen et al, who presented initially with pathologic evidence of PM, had Stage IVA-IVB with N2b-N3 nodal disease.13In the report by Harada et al, PG involvement with oral cavity cancers also appeared to directly correlate with the number of involved cervical nodes.12
Given the difficulty of salvaging a patient successfully with a locoregional recurrence (LRR) after primary radiation, and that PM results in poor prognosis, we believe all efforts should be made to address all known clinical and potential sub-clinical disease at the time of the initial curative treatment. Thus, in the setting of bulky or diffuse lymphadenopathy such as significant upper level II involvement in nasopharynx primaries or N2b-N3 disease in non-nasopharyngeal primaries, consideration should be paid to include the ipsilateral parotid in the CTV, even in the absence of radiologic involvement. In such cases, we would recommend that the PG be included in the low-risk CTV, which typically receives 54-56 Gy over 32-35 fractions using IMRT. An alternative strategy may be to compromise and avoid defining the ipsilateral parotid either as an organ-at-risk or as a target, thus providing moderate “incidental” dose to the organ.
Since the rarity of these cases precludes a systematic evaluation regarding the clinical factors (eg, number and size of LNs, presence of extracapsular spread, etc), decisions to include the PG in the CTV need to be made on a case-by-case basis for the present. The concern for ablating the ipsilateral PG function should be tempered by the desire to prevent recurrence, as well as the growing awareness that many other factors aside from parotid dose may affect QOL and xerostomia, including submandibular gland dose and oral cavity/minor salivary gland mean dose.14, 15Finally, with massive involvement of the cervical nodes, substantial sparing of the PG ipsilaterally is often not achievable due to the need to cover the level II lymphatics to the base of skull.
In summary, we believe that the prudent measure is to strongly consider including the PG in patients with massive level II lymphadenopathy. Our standard of care has recently been changed to reflect the findings reported here.
References:
- Cooper JS, Fu K, Marks J, et al. Late effects of radiation therapy in the head and neck region.Int J Radiat Oncol Biol Phys.1995;31:1141-1164.
- Bjordal K, Kaasa S, Mastekaasa A. Quality of life in patients treated for head and neck cancer: a follow-up study 7 to 11 years after radiotherapy.Int J Radiat Oncol Biol Phys.1994;28:847-856.
- Sher DJ, Neville BA, Chen AB, et al. Predictors of IMRT and conformal radiotherapy use in head and neck squamous cell carcinoma: a SEER-Medicare analysis.Int J Radiat Oncol Biol Phys.2011;81:e197-206. doi: 10.1016/j. ijrobp.2011.02.007.
- Cannon DM, Lee NY. Recurrence in region of spared parotid gland after definitive intensity-modulated radiotherapy for head and neck cancer.Int J Radiat Oncol Biol Phys.2008;70:660-665.
- Chao KS, Majhail N, Huang CJ, et al. Intensity-modulated radiation therapy reduces late salivary toxicity without compromising tumor control in patients with oropharyngeal carcinoma: a comparison with conventional techniques.Radiother Oncol.2001;61:275-280.
- Lee NY, de Arruda FF, Puri DR, et al. A comparison of intensity-modulated radiation therapy and concomitant boost radiotherapy in the setting of concurrent chemotherapy for locally advanced oropharyngeal carcinoma.Int J Radiat Oncol Biol Phys.2006;66:966-974.
- Dandekar V, Morgan T, Turian J, et al. Patterns-of-failure after helical tomotherapy-based chemoradiotherapy for head and neck cancer: implications for CTV margin, elective nodal dose and bilateral parotid sparing.Oral Oncology.2014;50:520-526. doi: 10.1016/j.oraloncology.2014.02.009.
- Chen AM, Farwell DG, Luu Q, et al. Marginal misses after postoperative intensitymodulated radiotherapy for head and neck cancer.Int J Radiat Oncol Biol Phys.2011;80:1423-1429. doi: 10.1016/j.ijrobp.2010.04.011.
- Harari PM. Beware the swing and a miss: baseball precautions for conformal radiotherapy.Int J Radiat Oncol Biol Phys.2008;70:657-659. doi: 10.1016/j. ijrobp.2007.10.065.
- Mendenhall WM, Mancuso AA. Radiotherapy for head and neck cancer--is the “next level” down?Int J Radiat Oncol Biol Phys.2009;73:645-646. doi: 10.1016/j. ijrobp.2008.08.061.
- Ng SH, Chang JT, Chan SC, et al. Nodal metastases of nasopharyngeal carcinoma: patterns of disease on MRI and FDG PET.Eur J Nucl Med Mol Imaging.2004;31:1073-1080.
- Harada H, Omura K. Metastasis of oral cancer to the parotid node.Eur J Surg Oncol.2009;35:890-894. doi: 10.1016/j.ejso.2008.09.013.
- Olsen SM, Moore EJ, Koch et al. Oral cavity and oropharynx squamous cell carcinoma with metastasis to the parotid lymph nodes.Oral Oncology.2011;47:142-144. doi: 10.1016/j.oraloncology.2010.11.010.
- Little M, Schipper M, Feng FY, et al. Reducing xerostomia after chemo-IMRT for head-and-neck cancer: beyond sparing the parotid glands.Int J Radiat Oncol Biol Phys.2012;83:1007-1014. doi: 10.1016/j.ijrobp.2011.09.004.
- Wang ZH, Yan C, Zhang ZY, et al. Impact of salivary gland dosimetry on post- IMRT recovery of saliva output and xerostomia grade for head-and-neck cancer patients treated with or without contralateral submandibular gland sparing: a longitudinal study.Int J Radiat Oncol Biol Phys.2011;81:1479-1487. doi: 10.1016/j. ijrobp.2010.07.1990.
- Mendenhall WM, Million RR, Mancuso AA, et al. Management of Head and Neck Cancer: A Multidisciplinary Approach. Second ed. Philadelphia, PA: J.B. Lippincott Co.; 1993.
- Rouviere H. Anatomie Des Lymphatiques de L’Homme. Paris, Fr: Masson Et C.; 1932.
- Conley J, Arena S. Parotid gland as a focus of metastasis. Arch Surg. 1963;87:757- 764.
- Ord RA, Ward-Booth RP, Avery BS. Parotid lymph node metastases from primary intra-oral squamous carcinomas.Int J Oral Maxillofac Surg.1989;18:104-106.
- Pisani P, Krengli M, Ramponi A, et al. Metastases to parotid gland from cancers of the upper airway and digestive tract.Br J Oral Maxillofac Surg.1998;36:54-57.
- Yarington CT, Jr. Metastatic malignant disease to the parotid gland.Laryngoscope.1981;91:517-519.

Biomarker Testing Paves the Way for Better Targeted Therapies in NSCLC
April 16th 2024At a live virtual event, Edward S. Kim, MD, MBA, discussed the evolving landscape of biomarker testing before making treatment decisions for patients with early-stage non–small cell lung cancer (NSCLC).
Read More
Creating Solutions for a 'Continual State of Transition' in Cancer Care
April 15th 2024In a Peers & Perspectives in Oncology feature article, we focus on the importance of the transition-of-care process for patients with cancer as they move from the inpatient to outpatient setting, as well as between lines of therapy with comments from Marc J. Braunstein, MD, PhD, and Michael Shusterman, MD.
Read More