Next Generation Diagnostics for Immuno-Oncology
Unlike traditional diagnostics that measure the presence, absence, or altered levels of a single analyte, immuno-oncology diagnostics seek to coalesce large amounts of immunological and tumor information into "signatures" that can be used to guide patient care.
Abstract
Current immuno-oncology therapies, although promising in terms of response duration, are effective only in a minority of patients, and current biomarkers of immune response have suboptimal specificity and sensitivity. Unlike traditional diagnostics that measure the presence, absence, or altered levels of a single analyte, immuno-oncology diagnostics seek to coalesce large amounts of immunological and tumor information into “signatures” that can be used to guide patient care. The only immuno-oncology biomarker on the market approved to guide administration of anti-programmed cell death protein 1 (PD-1) inhibitors is programmed death-ligand 1 (PD-L1) expression in the tumor measured by immunohistochemistry (IHC). However, its adoption is hampered by low accuracy and analytic challenges, including subjective interpretation. In this review, we identify features of an ideal immuno-oncology diagnostic, summarize the state of PD-L1 measurement by immunohistochemistry, and provide an overview of different biomarker platforms in clinical development that may guide patient decisions in the immuno-oncology field in the future.
Introduction
Rapid advances in our understanding of the fundamental biology of cancer and the integral role of the immune response to tumor progression are changing drug development and clinical practice. New therapies on the market and in development are offering the real promise of a cure to patients who previously had exhausted all known treatments. Checkpoint inhibitors, which disrupt negative signaling pathways in T cells, have seen recent clinical success as single agents in some solid tumors. However, outside melanoma and a subset of Hodgkin lymphoma, the vast majority of patients with metastatic solid tumors do not respond to checkpoint inhibitors, and combinations are more effective but can be more toxic and expensive. Therefore, optimal immuno-therapeutic drug development requires biomarker support for both mechanistic insight and patient selection. Unfortunately, the development of diagnostics and biomarkers predictive of response have not kept pace with drug discovery, further inhibiting the development of new therapeutics due to the inability to rationally select and monitor patients. This article will characterize the traits of an ideal immuno-oncology diagnostic, summarize the current diagnostic landscape, highlight unmet needs, and review promising new diagnostic technologies.
The Ideal Immuno-Oncology Diagnostic
A perfect immuno-oncology diagnostic must meet a number of different criteria: it must be sensitive, accurate, robust, and broadly applicable to different tumor types. Ideally, it should provide information about the factors that shape the interaction between tumor and the accompanying immune response.
Sensitivity: Analytical sensitivity represents the smallest amount of analyte of interest in a sample that can accurately be measured by an assay. In immuno-oncology, a test must be able to detect signals associated with the presence or absence of a tumor immune response from a much larger input of signal associated with tumor and the normal tissue. This requires highly sensitive molecular platforms such as the NanoString nCounter platform, Adaptive BioTechnologies T receptor (TCR) immune-profiling, and next-generation sequencing.
Accuracy: Analytical specificity is the ability of an assay to measure a particular analyte in the presence of other analytes in a sample. Diagnostic technologies have the potential to introduce analytic errors as the material is processed for analysis. For example, real-time polymerase chain reaction (PCR)-based diagnostics may introduce errors during enzymatic processing such as variations in amplicon efficiency during the PCR. In immunohistochemistry-based diagnostics, incomplete antigen retrieval can artificially obscure antibody binding sites, and suboptimal primary antibodies may not detect relevant isoforms or common variants of the analyte. Furthermore, secondary antibodies or visualization agents used in incorrect concentrations can reduce the signal-to-noise ratio by either dampening the positive signal or increasing the background staining. In-situ hybridization-based diagnostics are subject to false negative errors if the denaturing reactions are not performed to completion, and false positive errors can be introduced if the probes are not specific for the sequence of interest. An ideal diagnostic must be able to detect the analyte of interest accurately without the introduction of false-positive or false-negative readouts.
Robustness: A diagnostic should be resilient against variations in data interpretation so that results are quantitative, not subjective, and the same sample run in different labs will generate the same results.
The specific genetic and epigenetic changes that arise within the tumor are unique to each tumor and even within a single tumor. Metastases differ from the primary tumor due to random mutation and the effects of existing within different environmental niches. Furthermore, the gene and protein expression is a dynamic process that changes with time. Thus, a single biopsy may not capture all critical information. An ideal diagnostic would integrate multiple signals into robust signatures that are buffered against changes of a single analyte and reflect the fundamental biology used by the tumor to grow and persist in the face of an active immune response.
Broad Applicability: Tests that characterize the disease status from an immunological point of view have broader clinical applicability for the immuno-oncology field and will inform a broad range of therapies than tests that focus on the mechanism of action of a single drug. Profiling immunological consequences of intervention will be more practical than offering multiple tests for different drugs, each with their own reagents, protocols, and interpretation guidelines.
The Current Immuno-Oncology Diagnostics
The first checkpoint inhibitors to be developed in conjunction with diagnostics are the programmed cell death protein 1 (PD-1)-targeting antibodies nivolumab (Opvido) and pembrolizumab (Keytruda). Other agents targeting the same pathway are in late-stage development and are expected to become commercially available in the near future(TABLE 1). Although the two commercially available monoclonal antibodies (mAbs) share the target and mechanism of action, their current indications for use are not identical, reflecting the different clinical development plans. They are both approved in advanced melanoma as single agents, and nivolumab is also approved in melanoma in combination with ipilimumab (anti-cytotoxic T-lymphocyte-associated protein 4 [CTLA-4]). Both are approved in nonsmall cell lung cancer (NSCLC), although pembrolizumab indication is limited to patients whose tumors express programmed death-ligand 1 (PD-L1) by immunohistochemistry (IHC); nivolumab has also been approved in renal cell cancer.
There are nine drugs in development targeting the PD-1/PD-L1 pathway, and the current practice of pharmaceutical companies is to independently develop an anti-PD-L1 IHC diagnostic assay.1Therefore, if each therapeutic drug was approved in conjunction with a companion diagnostic one, the matrix of therapeutics and diagnostics would present a complex challenge for testing and decision-making in the clinic. In addition, the purpose of each assay has been shaped by clinical experience. As a result, the PD-L1 IHC 22C3 pharmDx, which was used as an inclusion criteria for patient enrichment in advance NSCLC trials with pembrolizumab, is required for clinical use of the drug in this indication, whereas the PD-L1 IHC 28-8 pharmDx, retrospectively evaluated in the same patient population, is used to inform on the risk-benefit assessment for different patient subgroups as defined by the biomarker positivity.
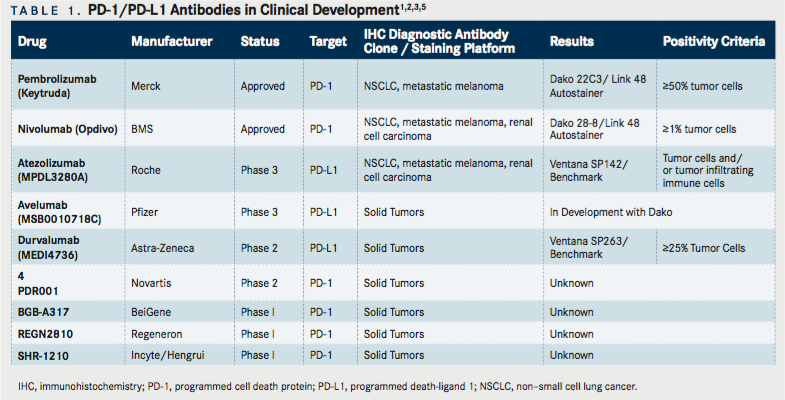
Compounding the issues with the current PD-L1 IHC assays, evaluating PD-L1 as a single analyte biomarker is less than ideal. Cellular, spatial, and temporal heterogeneity all contribute to the poor prediction accuracy of this biomarker in the clinic (ie, lack of both positive and negative predictive value), as it has been shown that the majority of PD-L1+ tumors fail to respond to a PD-1 blockade, and a subset of patients whose tumor biopsies are PD-L1 achieve clinical benefit.2TABLE 1summarizes the PD-1 and PD-L1 antibodies currently in clinical development together with a companion diagnostic.
Clearly, the existing diagnostics that rely solely on measuring PD-L1 expression in the tumor environment are suboptimal for informing treatment decisions regarding treatment PD-1 pathway blockades. The multiplicity of antibodies being used to target the PD-1/PD- L1 pathway, the requirement for a clinical lab to select a single staining platform or to adopt multiple platforms, and the need for a pathologist to review patient samples and render a subjective judgement all impair the efficacy of these assays. This is further compounded by the wide range of values that constitute “PD-L1 positivity” associated with each test. There is no consensus in the literature about what degree of PD-L1 expression is adequate to elicit biological activity, and therefore, each test has its own cut-offs. Overall, there is evidence that higher levels of PD-L1 expression correlate to better response to PD-1 blockades.
In the clinical trial for pembrolizumab in advanced NSCLC, patients whose tumors were at least 50% positive had better overall survival and progression-free survival, but there was minimal difference in outcomes between patients whose tumors were <1% or 1-49% PD-L1+2. For nivolumab, for which PD-L1 IHC was developed as a complementary diagnostic and is not required for drug prescribing, the cut-off for PD- L1 positivity is much lower (1% of tumor cells), and for durvalumab is intermediate at 25%.5Scoring for atezolimumab is unique, because it considers PD-L1 expression on both tumor cells and immune cells to generate a score.5Despite the most restrictive cutoffs for PD-L1 positivity (ie, 50%), response rates for pembrolizumab in advanced NSCLC are approximately 40%, indicating that the biology of immune response is more complicated than previously believed, and additional work needs to be done to understand how the degree of PD-L1 expression affects the tumor-immune response.
Furthermore, that complexity exists entirely within diagnostics developed for a single immune checkpoint axisPD-1 and PD-L1. The other approved immune checkpoint inhibitor for treatment of melanoma, ipilimumab (Yervoy), a CTLA-4 blocking antibody, does not have an accompanying diagnostic. CTLA-4 is a central negative regulator of T cell activation, and CLTA-4 blockades induce profound T cell activation and accompanying immunotoxicity that can be dose-limiting in some patients.6Additionally, CLTA-4 blockades are only efficacious in a minority of patients. Therefore, a companion or complementary diagnostic with predictive power to identify patients likely to respond would be extremely informativepatients who are likely to respond could enter treatment with greater confidence that the treatment will be beneficial, and patients unlikely to benefit from the drug could be spared the side effects and cost in favor of another treatment plan. However, a companion diagnostic to accompany ipilimumab therapy would be even less straightforward to develop than an anti-PD-L1 diagnostic, as CTLA-4-mediated suppression occurs in secondary lymphoid organs rather than at the site of the tumor, and the ligands for CTLA-4, namely CD80 and CD86, which are expressed on antigen presenting cells, are also the ligands for the T cell costimulatory receptor CD28.7Consequently, their expression may not always correlate with immune suppression. Therefore, development of an ipilimumab companion diagnostic would be complicated by the need to select the appropriate marker and profile non-tumor tissue.
Beyond CLTA-4 and PD-1/PD-L1, other checkpoint inhibitors are rapidly being advanced to the clinic setting and will likely require new diagnostics for rational use. Additional immuno-oncology approaches are also in development, including cancer vaccines, adoptive cell therapy with chimeric antibody receptor expressing T cells (CAR-T), small molecule modulators of immune response (e.g. TLR agonists), and nucleic acid-based therapies. These potential treatments will need diagnostics to select patients and biomarkers to monitor immune responses. This critical need for new diagnostic solutions has led to the development of a number of new technologies or redeployment of existing technologies as alternative diagnostic platforms for the immuno-oncology field.
Next Generation Immuno-Oncology Diagnostics
NanoString nCounter Platform: The nCounter platform utilizes multiplexed optically barcoded deoxyribonucleic acid (DNA) oligos and direct hybridization to DNA or ribonucleic acid (RNA) target sequences coupled with digital counting to quantify the target within a sample without amplification(FIGURE 1). The sample processing is minimal and the technology is extremely tolerant of variations in the quality of input material, rendering the technique well-suited for adoption in the clinical laboratory. The platform is flexible, and can measure up to 800 targets at once. The assay is straightforwardsample is hybridized to two 50 base pair probes via complementary sequence annealing in solution(FIGURE 1A). The capture probe is used to affix the target/probe complex to the surface of the nCounter cartridge. The reporter probe is labeled with a fluorescent barcode that uniquely identifies the bound target. Once the complex is immobilized to the surface of the cartridge, the nCounter Digital Analyzer images and counts the barcodes associated with each target, generating a data file listing the relative number of counts for each targeted gene or protein(FIGURE 1B, C). The platform is compatible with a wide variety of sample inputs, including formalin-fixed, paraffin-embedded (FFPE) tissue (1-2 5 μm sections), fresh or fixed cells (5000), and purified RNA (100ng). Data analysis and graphing can be performed by the investigator using the nSolver analysis suite.
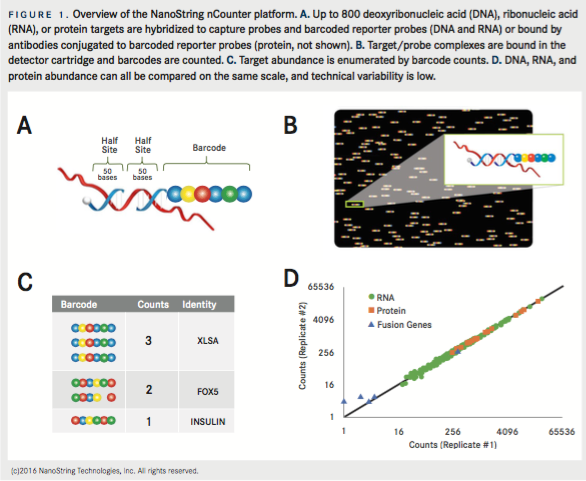
The nCounter system is able to measure many different biological phenomenon from DNA and RNA, including copy number variation, gene fusion events, single nucleotide variants, gene expression, and miRNA expression. Recent developments in the platform enable quantitation of proteins in addition to DNA and RNA by conjugating the barcoded oligos to antibodies that are subsequently used for bind protein targets of interest. Protein detection is currently available for peripheral blood mononuclear cells, dissociated tumor tissue, or cultured cells. From these cells, DNA, RNA, and protein can be detected from the same sample in the same hybridization reaction and results visualized in unison on the same graph(FIGURE 1D). Technical variability on the nCounter is minimal between different users and even between different labs because no amplification is required, and biological replicates routinely have a coefficient of determination (R2) of greater than 0.9(FIGURE 1D). One limitation of the nCounter assay is that target detection is aggregated across the sample rather than being traceable to one or more cell types, which precludes analysis of how expression of a given target within a single cell affects the biology of the system.
The nCounter platform (nCounter Dx Analysis System) has already received FDA clearance for use with the Prosigna assay, a multiplexed gene expression assay based on the PAM50 gene signature, which estimates a risk of distant recurrence-free survival for patients with hormone receptor positive, lymph node-negative or lymph node-positive (1-3 positive nodes) breast cancer.8The Prosigna assay has seen worldwide adoption, is recognized by all major oncology guidelines (eg,National Comprehensive Cancer Network [NCCN], American Society of Clinical Oncology [ASCO], European Society for Medical Oncology [ESMO], etc.) and is reimbursed by an increasing number of payers. In addition to the Prosigna assay application, the nCounter platform is robust and flexible enough to also build diagnostic tests for immuno-oncology. As early evidence of the power of this approach in this field, NanoString has recently entered into a co-development agreement with Merck to build an improved companion diagnostic for pembrolizumab (Keytruda) to predict patient responses based upon immune gene expression signatures.9This is the first step in the development of a more “universal” immuno-oncology diagnostic panel that could provide predictive information about multiple immuno-oncology therapeutic interventions at the level of the single patient.
HalioDx Immunoscore: Immunoscore is a measurement of the lymphocytic infiltrate into tumors based upon immunohistochemistry staining and digital pathology to quantify T cells (CD3+), cytolytic T cells (CD8+), and memory T cells (CD45RO+).10Strong evidence exists that high densities of T cell infiltrates into the tumor are associated with prolonged disease-free survival and overall survival.11,12Immune infiltrates with the respective markers are quantified both at the tumor core and at the invasive margin, and normalized counts per area are summed and categorized onto a combined 5-point scale. One limitation of the Immunoscore is that it provides minimal information about T cell phenotypes and can provide only gross level information about the nature of the immune response.13For example, it does not distinguish T cells of non-CD8 phenotype, so an immune infiltrate comprised predominantly of Th1 CD4+ T cells that support anti-tumor activity would look identical to one comprised of Th2 or regulatory CD4+ T cells, which inhibit anti-tumor activity. Even within the CD8 T cell population, subpopulations exist that have greater or lesser cytolytic activity, and these nuances of the immune response are not provided by the Immunoscore
The Immunoscore is being commercialized into a complementary diagnostic by HalioDx as a prognostic assay, and the test for colon cancer application is predicted to be released in 2016. Recent publications suggest that there may be a better predictor of clinical prognosis in colon tumors than the classic tumor/node/metastasis (TNM) staging, or microsatellite instability.14Additionally, the prognostic value of the Immunoscore has also been shown more recently to extend to hepatocellular carcinoma and NSCLC.15,16
Adaptive BioTechnologies ImmunoSEQ: Adaptive Bioscience has developed the immunoSEQ platform for deep nucleic acid sequencing that can be applied to profiling T and B cell diversity within the tumor.17The complementary determining region 3 (CDR3) region of the TCR or B cell receptor (BCR) is unique to each cell as a result of gene rearrangement during cell development to increase the diversity of the repertoire. A combination of PCR and next-generation sequencing is used to define the genetic sequence of the CDR3 region from each cell. Evidence suggests that in melanoma and ovarian tumors, an increase in immune cell repertoires can correlate with better patient prognoses, and the same increase in T cell clonality may also correlate with response to immunotherapy.18,19One limitation is that TCR/BCR sequencing does not give information about the activation status of the lymphocyte or insights into which epitopes are being recognized.20
Next Generation Sequencing (NGS): The principles of deep DNA sequencing have multiple applications in the oncology setting, including quantification of the mutational load within a tumor. Studies have demonstrated that tumors induced by exposure to mutagens or associated with deficiencies in DNA repair more frequently have high levels of mutations than do tumors of other etiological origins.21,22. Elevated mutational load has been shown to be associated with increased tumor infiltration by lymphocytes and enhanced responses to immunotherapy.23,24,25Several organizations have developed NGS-based diagnostics that profile the mutational load in tumors. Foundation Medicine has developed the FoundationOne test, which uses a targeted sequencing approach to characterized mutations in 315 genes known to be mutated in solid tumors.26Similarly, both the miSeqDX (Illumina) and the Ion PGM (Thermo Fisher Scientific) have received FDA clearance as diagnostics platforms for the development of in-vitro diagnostic assays by clinical labs.27,28To date, the majority of NGS diagnostics in development focus on characterizing mutations from specific genes that are known cancer drivers rather than assessing the overall mutational burden, but as the cost and complexity of NSG sequencing continues to fall, broader interrogation will be enabled.
Another application of NGS is to monitor for minimal residual disease (MRD). In a technology utilized by multiple companies (including Adaptive BioTechnologies, Illumina, Thermo Fisher, and others), NGS approaches can be used to monitor for MRD and outgrowth of the tumor based upon expansion of cancer clones with known mutations. Originally, MRD monitoring was done using quantitative PCR of immunoglobulin and T cell receptor genetic loci or by multicolor flow cytometry.29However, these techniques were difficult to perform consistently or lacked the sensitivity needed for clinical utility. In the protocol used today, cancer clones are identified from a known tumor sample, and sequenced for indicative mutations in the T cell receptor or immunoglobulin genes. Subsequent patient samples are sequenced again and monitored for expansion of the mutation-bearing tumor cells, which would indicate outgrowth of the tumor. This technique is well-suited to monitoring patients with leukemias, lymphomas, or multiple myelomas. This technique is highly sensitive for detection of rare cell populations, but provides no information about the immune status of the patient. In addition to hematological malignancies, the technique can also be applied to other tumors by monitoring blood for circulating tumor cells. One disadvantage of this technique is that sample processing and data analysis are not trivial and are usually done by central labs that can have extended turnaround times.
Conclusion
The landscape of immuno-oncology diagnostics is changing rapidly, and new technologies are enabling researchers and clinicians to monitor ongoing immune responses in ways never before possible, with the goal of obtaining more information relevant to each patient’s potential outcome. There remains a great deal of uncertainty in the field as consensus is reached about best platforms, best practices, and best reagents. The characteristics of an ideal companion/complementary diagnostic are in some cases mutually exclusive, so it is clear that any technology developed will have limitations. As the practicing oncology community waits for consensus on a recommended path forward, diagnostic developers will continue to advance their technologies as rapidly as possible. New technologies will drive the diagnostics field to generate improved tests; they will become more sensitive, more accurate, more robust, and more applicable to many kinds of cancer and immunotherapeutic intervention. Oncologists must be cautious and prudent with their patients’ care, but also proactive in finding and implementing new technologies that improve outcomes. As all stakeholders participate in advancing diagnostics development and adoption, the burden of cancer for patients will be reduced.
References
- U.S. National Institutes of Health. https://clinicaltrials.gov/. Accessed March 14, 2016.
- Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer.New Engl J Med. 2015; 372(21): 2018-2028. doi: 10.1056/ NEJMoa1501824.
- Scholl LM, Aisner DL, Allen TC, et al. Programmed death ligand 1 immunohistochemistrya new challenge for pathologists.Arch Pathol Lab Med. 2016. Early online release. http://dx.doi.org/10.5858/arpa.2015-0506-SA.
- He J, Hu Y, Hu M, Li B. Development of PD-1/PD-L1 pathway in tumor immune microenvironment and treatment for non-small cell lung cancer.Sci Rep. 2015; 5:13110. doi:10.1038/srep13110.
- Kerr KM, and Nicolson MC. Non-small cell lung cancer, PD-L1, and the pathologist.Arch Pathol Lab Med. 2016;140(3):249-254. doi: 10.5858/arpa.2015- 0303-SA.
- Wolchok JD, Hodi FS, Weber JS, et al. Development of ipilimumab: a novel immunotherapeutic approach for the treatment of advanced melanoma.Ann N Y Acad Sci. 2013;1291:1-13. doi: 10.1111/nyas.12180.
- Daud A. Current and emerging perspectives on immunotherapy for melanoma.Semin Oncol. 2015;42 Suppl 3:S3-S11. doi: 10.1053/j.seminoncol.2015.10.003.
- Prosigna [package insert]. Seattle, WA: NanoString Technologies; 2015.
- Merck and NanoString announce clinical research collaboration to develop an immune-related gene expression assay for use in the development program for KEYTRUDA® (pembrolizumab) [press release]. Seattle WA: NanoString Technologies; May 28, 2015. http://investors.nanostring.com/releasedetail.cfm?releaseid=915259. Accessed March 16, 2016.
- Galon J, Mlecnik B, Bindea G, et al. Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours.J Path. 2014; 232(2):199-209. doi: 10.1002/path.4287.
- Anitei MG, Zeitoun G, Mlecnik B, et al. Prognostic and predictive values of the immunoscore in patients with rectal cancer.Clin Cancer Res. 2014; 20(7):1891-1899. doi: 10.1158/1078-0432.CCR-13-2830.
- Galon J, Costes A, Sanchez-Cabo F, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome.Science. 2006; 313(5795): 1960-1964.
- Galon J, Angell HK, Bedognetti D, Marincola FM. The continuum of cancer immunosurveillance: prognostic, predictive, and mechanistic signatures.Immunity. 2013;39(1):11-26. doi: 10.1016/j.immuni.2013.07.008.
- Mlecnik B, Bindea G, Angell HK, et al. Integrative analyses of colorectal cancer show immunoscore is a stronger predictor of patient survival than microsatellite instability.Immunity. 2016;44(3):698-711. doi: 10.1016/j.immuni.2016.02.025.
- Gabrielson A, Wu Y, Wang H, et al. Intratumoral CD3 and CD8T-cell densities associated with relapse free survival in HCC.Cancer Immunol Res. 2016; Mar 11. Early online release.
- Cooper ZA, Frederick DT, Juneja VR et al. BRAF inhibition is associated with increased clonality in tumor-infiltrating lymphocytes.Oncoimmunology. 2013;2(10):e26615.
- Adaptive Biotechnologies. http://www.adaptivebiotech.com/immunoseq. Accessed April 6, 2016.
- Emerson RO, Shewood AM, Rieder MJ, et al. High-throughput sequencing of T cell receptors reveals a homogeneous repertoire of tumor-infiltrating lymphocytes in ovarian cancer.J Pathol. 2013;231(4):433-440. doi: 10.1002/path.4260.
- Tumeh PC, Harview CL, Yearley JH, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance.Nature. 2014;515(7528):568-571. doi: 10.1038/nature13954.
- Klinger, Pepin, Wilkins, et al. Multiplex identification of antigen-specific T cell receptors using a combination of immune assays and immune receptor sequencing.PLoS One. 2015;10(10):e0141561. doi: 10.1371/journal. pone.0141561
- Alexandrov LB, Nik-Zainal S, Wedge DC, et al. Signatures of mutational processes in human cancer.Nature. 2013;500(7463):415-421. doi: 10.1038/nature12477.
- Lawrence MS, Stonjanov P, Polak P, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes.Nature. 2013;499(7457):214-218. doi: 10.1038/nature12213.
- Brown SD, Warren RL, Gibb EA, et al.Neo-antigens predicted by tumor genome meta-analysis correlate with increased patient survival.Genome Res. 2014; 24(5): 743-750. doi: 10.1101/gr.165985.113.
- Rizvi NA, Hellmann MD, Snyder A, et al. Mutational landscape determines sensitivity to PD-1 blockade in nonsmall cell lung cancer.Science. 2015;348(6230):124-128. doi: 10.1126/science.aaa1348.
- Snyder A, Makarov V, Merghoub T, et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma.N Engl J Med. 2014;371(23):2189-99. doi: 10.1056/NEJMoa1406498. Accessed March 18, 2016.
- Foundation Medicine. http://foundationone.com/learn.php. Accessed March 18, 2016.
- Thermo Fisher Scientific Announces Listing of the Ion PGM Dx System with the U.S. FDA as class II medical device [press release]. Carlsbad, CA: ThermFisher Scientific. Sept. 18, 2014. http://news.thermo sher.com/press-release/life-technologies/thermo-fisher-scientific-announces-listing-ion-pgm-dx-system-us-fda-. Accessed March 18, 2016.
- Illumina. http://www.illumina.com/systems/miseqdx/system.html. Accessed March 18, 2016.
- van Dogen JJM, van der Velden VHJ, Brüggemann M, Orfao A. Minimal residual disease diagnostics in acute lymphoblastic leukemia: need for sensitive, fast, and standardized technologies.Blood. 2015;125(26):3996-4009. doi: 10.1182/blood-2015-03-580027.

Biomarker Testing Paves the Way for Better Targeted Therapies in NSCLC
April 16th 2024At a live virtual event, Edward S. Kim, MD, MBA, discussed the evolving landscape of biomarker testing before making treatment decisions for patients with early-stage non–small cell lung cancer (NSCLC).
Read More