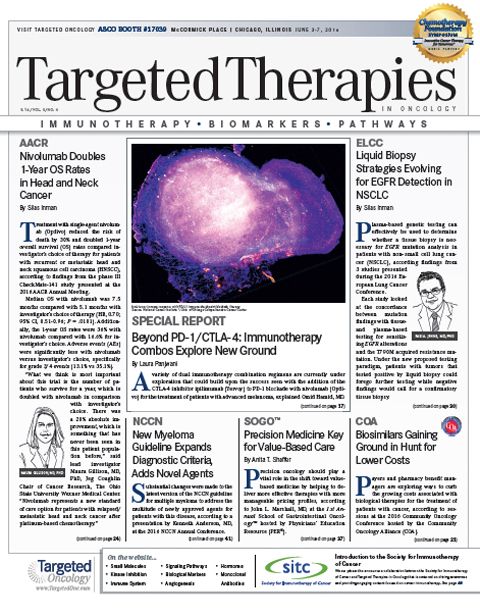
Biosimilars Gaining Ground in Hunt for Lower Costs
Payers and pharmacy benefit managers are exploring ways to curb the growing costs associated with biological therapies for the treatment of patients with cancer.
Jim Koeller, PharmD
Payers and pharmacy benefit managers are exploring ways to curb the growing costs associated with biological therapies for the treatment of patients with cancer, according to sessions at the 2016 Community Oncology Conference hosted by the Community Oncology Alliance (COA).
A recent report commissioned by COA showed a 335% increase in Medicare spending from 2004 to 2014 for biologics. For commercial payers, this increase was 485%. Spending on biologics increased more than any other category in the report, and the only expense that decreased was for other types of cancer drugs and chemotherapy, besides biologics, cytotoxics, and radiation.
With this dramatic increase in spending, biosimilars have been welcomed with open arms from those who feel they may lower costs. There are now 2 biosimilars approved in the United States, with a growing number expected to enter the market across a broad range of therapeutic areas within the next few years.
As a host of biosimilars rush toward approval, several questions remain regarding the efficacy, comparability, and tolerability of these agents. Moreover, despite the focus in this area, there is debate as to whether biosimilars are capable of reducing overall costs. The first approved biosimilar, filgrastim-sndz (Zarxio), debuted at a discount of just 15%.
At the COA meeting, Jim Koeller, PharmD, professor, University of Texas at Austin & the Health Science Center, moderated a panel discussion on the development process for biologics. The panel included key voices from the pharmaceutical companies developing these agents, including Amgen, Genentech, Sandoz Biopharmaceuticals, and EMD Serono. In the discussion, each panelist gave an overview of different aspects of the biosimilar development process.
The first point that was emphasized was that biosimilars are not comparable to generics, since the manufacturing process is far more complex. In general, biologics are 500 times smaller than generics. Additionally, the agents are manufactured using living cells and then go through a purification process. Each step in this process provides the opportunity for error. The generic process involves one step of chemical synthesis.
“What we understand is biosimilars are not generics. It needs reverse engineering back to the innovator biologic,” said Sue Caleo-Naeyaert, senior director Biosimilars Policy, Merck Serono. “Biologics are never the same, and they are very different from genericsthese variability can occur from batch to batch production. Even slight changes in the manufacturing process, to improve the product, results in changes in the final product,” she explained.
The current wave of biosimilar is due in part to an abbreviated licensure pathway that was established in 2010 under the Affordable Care Act. This was created under a law known as the Biologics Price Competition and Innovation Act, in an attempt to lower costs.
“The objective was to allow continued innovation but also allow cheaper copies of already-approved biological,” said Earl Dye, PhD, director, Technical Regulatory Policy, Genentech. “The abbreviated approval process has lower submission requirements of preclinical and clinical data for FDA review.”
The approval application for a biosimilar requires proof of quality, safety, and efficacy. The FDA will only approve biosimilars with proven high similarity to an FDA-approved biological product. There must be no clinically meaningful differences in safety and efficacy, and, if a new indication is sought outside of the reference products, additional studies must be conducted.
“Unlike the extensive 3-phase clinical studies required by the company that develops the innovator biological, the biosimilar developer does extensive functional comparison with the reference product and also some additional preclinical studies and clinical studies to show that any differences from innovator does not translate into significant clinical effect,” explained Dye.
Necessary data for a biosimilar approval can be from analytical studies, which show a high similarity between the two agents, and findings from animal studies or a clinical study or studies with endpoints focused on immunogenicity, pharmacokinetics, or pharmacodynamics. These studies do not have traditional endpoints for new drug development, such as overall survival or objective response rates.
“Biosimilar clinical studies are not designed or powered to conduct safety-efficacy studies,” according to Jim McKay, PhD, director, Clinical Development and Medical Affairs, Sandoz Biopharmaceuticals. “So the purpose of clinical studies for biosimilars is very different from that for reference product. While labels are mostly alike, slight differences may exist, such as indications for use.”
Interchangeability requires extra clinical data that proves that switching between the biosimilar and reference product will not affect efficacy or safety, according to McKay. An application for an interchangeable biologic requires additional data indicating that the biosimilar is capable of producing the same clinical result as the reference product. Interchangeable products may be substituted without permission from a prescribing healthcare provider.
“Pharmacovigilance is very important for biologicals overall,” said Thomas Felix, MD, director, R&D Policy, Amgen. “Biosimilar manufacturers need the ability to analyze safety of their products. There are issues of misattribution of adverse events, where even if use of originator product declines, adverse events are attributed to the originator.”
Naming of the follow-on products is also unclear. The FDA has released a draft naming guidance for biologics, which indicates the need for a hyphenated suffix, but “this is still being worked on,” Felix said. “There is also a global discussion involving the World Health Organization for standardizing a naming approach across countries, and that too is still being finalized,” he added.
Powell Reviews Updated IO/TKI Data and AE Management in Endometrial Cancer
April 18th 2024During a Case-Based Roundtable® event, Matthew A. Powell, MD, discussed the case of a patient with advanced endometrial cancer treated with lenvatinib plus pembrolizumab who experienced grade 2 treatment-related hypertension.
Read More
Savona Discusses First-Line JAK Inhibition for Patients With Myelofibrosis at Risk of Anemia
April 17th 2024During a Case-Based Roundtable® event, Michael Savona, MD, and participants discussed the case of a patient with myelofibrosis and moderate anemia receiving JAK inhibitor therapy.
Read More
Biomarker Testing Paves the Way for Better Targeted Therapies in NSCLC
April 16th 2024At a live virtual event, Edward S. Kim, MD, MBA, discussed the evolving landscape of biomarker testing before making treatment decisions for patients with early-stage non–small cell lung cancer (NSCLC).
Read More
Creating Solutions for a 'Continual State of Transition' in Cancer Care
April 15th 2024In a Peers & Perspectives in Oncology feature article, we focus on the importance of the transition-of-care process for patients with cancer as they move from the inpatient to outpatient setting, as well as between lines of therapy with comments from Marc J. Braunstein, MD, PhD, and Michael Shusterman, MD.
Read More