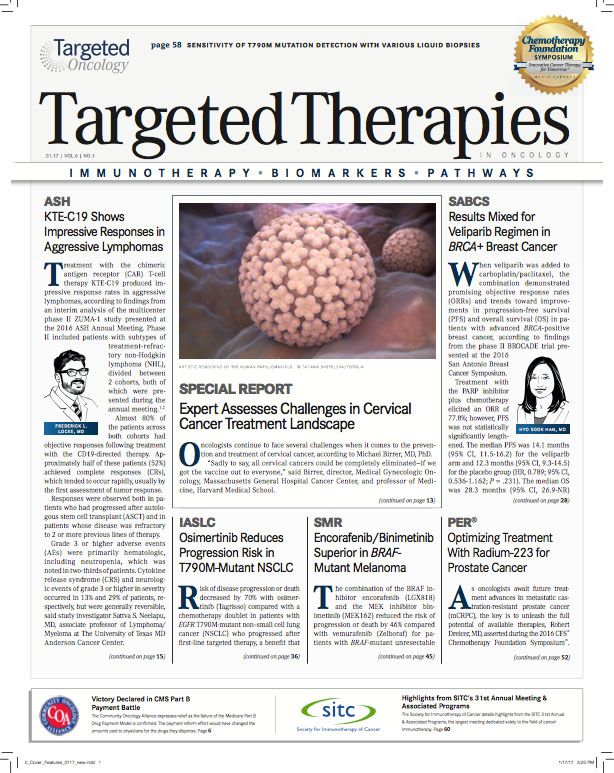
Optimizing Treatment With Radium-223 for Prostate Cancer
Robert Dreicer, MD, discusses ongoing developments in mCRPC, including the latest approaches with radium-223.
Robert Dreicer, MD
As oncologists await future treatment advances in metastatic castration-resistant prostate cancer (mCRPC), the key is to unleash the full potential of available therapies, Robert Dreicer, MD, asserted during the 2016 CFS Chemotherapy Foundation Symposium.
One agent that oncologist are focused on optimizing, Dreicer said, is radium-223 (Xofigo). Optimal use of this treatment remains mostly unknown, with current efforts focusing on exploring the agent’s potential in combination regimens.
For instance, a phase III trial is randomizing patients with bone predominant mCRPC to radium-223 plus abiraterone acetate (Zytiga) or abiraterone alone (NCT02043678). Additionally, a randomized phase IIa study is evaluating the efficacy and safety of radium-223 in combination with abiraterone or enzalutamide (Xtandi) in patients with mCRPC to investigate bone-scan response, radiological progression-free survival, overall survival, and skeletal events (NCT02034552).
In an interview withTargeted Therapies in Oncology(TTO), Dreicer, associate director, Clinical Research, and deputy director, University of Virginia Cancer Center, discussed ongoing developments in mCRPC, including the latest approaches with radium-223.
TTO:What are the next steps with radium-223?
Dreicer:
Radium-223 is a very unique agent, and it’s one of the 2 approved therapies in advanced prostate cancer that is not an AR- targeted therapy. It makes some intrinsic sense to take multiple different pathways to treat a disease, and therefore the combining of agents like abiraterone and enzalutamide with radium-223 is a very intriguing and appropriate set of studies to donot only because we’re trying to figure out if we can do better in terms of getting better responses, more prolonged responses, changed progression-free survival, things like that, but frankly also from an economic perspective. Before we start combining very expensive agents, we need some indication that there’s a rationale to do that. So it’s clearly an important thing to study. Are we anywhere close to knowing the answers to that? I don’t think so, but the studies are ongoing.
TTO:What are some ongoing studies with radium-223?
Dreicer:
A number of studies are being done, including retreatment studies, to look at more than 6 cycles of therapythe 6 being somewhat arbitrary. The retreatment paradigm is very intriguing, especially in patients who may have benefitted. Remember, one of the challenges with radium-223 is that there’s no objective antitumor activity. It’s a bone-targeted therapy; PSA responses are not common.
Therefore, radium-223 is still one of those therapies that we wonder how to optimally integrate into the management paradigm. And, because it’s bone-targeted, patients with more than minimal nodal disease really are not great candidates, so that’s another reason to think about combinatorial treatment. There are a lot of things about radium-223 that remain to be addressed, and I think its uptake in the community is still patchy. I think some of that is practice patterns, and understanding where it may be best applied, so more data will certainly help clinicians in the community to figure out when radium-223, or radium-223 combinations, may be best for their patients.
TTO:Anecdotally, how have you seen this agent specifically impact patients in terms of quality of life?
Dreicer:
I tend to use it in a pre-docetaxel setting. These are patients who meet the label, in terms of having some minimal to moderate pain.
Pain relief is a little hard to gauge. Again, many of these patients are not that symptomatic, and of course, all of our patients have osteoar- thritis. It’s a challenge, one that’s not typical when we compare it to challenges associated with sipuleucel-T (Provenge). There’s no real true way to understand objective antitumor activity.
Therefore, if you can treat someone with 6 cycles of therapy and their disease has not overtly progressed, is it because of or in spite of [the therapy]? We know from the randomized trial that there is a survival benefit. So, in a sense, when we use these therapies, because a pain endpoint was not baked into the randomized trial, it’s a little hard to tell a patient, “Look, we’re doing this to try to minimize your pain. What we’re trying to do is, we know that there’s a decrease in symptomatic skeletal events, and that there may be a survival benefit.” And I think that that’s how we approach patients today. I’d like more data to be able to be a bit more definitive.
TTO:Do you think that there will be a newer or second-generation version of radium-223? Is there going to be some competition there?
Dreicer:
That’s an interesting question. Because it’s a unique molecule, because of its sparing of the bone marrow and relatively well-tolerated profile, it lends itself to integration earlier in the disease course, where it’s going to be studied, and it lends itself to combinatorial therapies. I suspect we’re going to see more and more of this. It’s a bone-trophic disease, and therefore, there are going to be a lot of people thinking about this. Can you have a “better” radium-223? I don’t know the answer to that, so I think time will tell how this goes. But I think the future is likely in combinations of therapies, as opposed to radium-223 as a monotherapy.
TTO:What doyou think is important for community oncologists to take away from all of this?
Dreicer:
Right now, we’ve hit a little bit of a time delay in terms of the therapies that have been developed. Clearly, the next wave of therapies are DNA mismatch repair, and targeted therapies, but even that is only going to impact a quarter, perhaps, of patients with castration-resistant disease. It’s really about optimizing the therapies that we have, as we begin to think about new drugs or new combinations that may be able to push us down the road a little bit.
Immunotherapyother than sipuleucel-T—has not been widely used. The checkpoints have been a little slower in prostate cancer because early data weren’t as compelling, although recent data presented at ESMO suggested that looking at checkpoints or other combinations may be very reasonable in some subsets of patients.
Optimally using the drugs we have and guring out sequencing, which will be a clinical judgment until we get more datathat’s what we need to walk away with to provide better care for our patients.
Creating Solutions for a 'Continual State of Transition' in Cancer Care
April 15th 2024In a Peers & Perspectives in Oncology feature article, we focus on the importance of the transition-of-care process for patients with cancer as they move from the inpatient to outpatient setting, as well as between lines of therapy with comments from Marc J. Braunstein, MD, PhD, and Michael Shusterman, MD.
Read More