Ovarian Cancer Diagnosis, Time to Treatment Improved Since ACA
After passage of the Affordable Care Act, women with ovarian cancer who were pre-medicare-aged were more likely to be diagnosed at an early stage and receive treatment within 30 days of diagnosis compared to prior to the ACA, according to findings presented at the 2019 ASCO Annual Meeting.
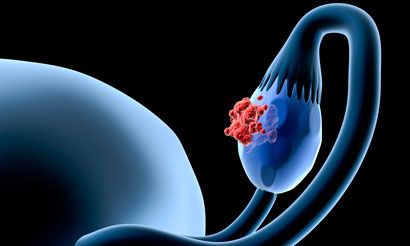
After passage of the Affordable Care Act (ACA), women with ovarian cancer who were pre-medicare-aged were more likely to be diagnosed at an early stage and receive treatment within 30 days of diagnosis compared to prior to the ACA, according to findings presented at the 2019 ASCO Annual Meeting.
Findings demonstrated a relative gain of 1.7% in early-stage (defined as stage I or II) diagnosis of ovarian cancer in women aged 21 to 64, compared with women ≥65, many of whom were presumed to be on Medicare. The 1.7% increase indicates that of the 22,000 women diagnosed annually, approximately 400 more have the potential to be diagnosed at a stage that is both early and treatable, thereby extending potential survival time, lead author Anna Jo Smith, MD, MPH, said.
The study also demonstrated an increase of 1.6% in women aged 21 to 64 treated within 30 days of diagnosis, compared with the control group.
Among publicly insured women aged 21 to 64, there were relative gains of 2.5% in both the diagnosis of ovarian cancer and time to treatment.
Smith, a resident in the Johns Hopkins Department of Gynecology and Obstetrics, at Baltimore, Maryland, and Amanda Nickles Fader, MD, director of the Kelly Gynecologic Oncology Service and an associate professor at Johns Hopkins, evaluated ovarian cancer data from the National Cancer Database, which records data on approximately 70% of all new ovarian cancer cases. They concluded that the ACA led to an increase in ovarian cancer treatment and more treatment occurring within 30 days of diagnosis, thereby increasing chances of survival for women with ovarian cancer.
“Detecting and treating ovarian cancer at an early stage saves lives and lowers healthcare costs compared with treatment of cancer at a more advanced, incurable stage,” said Smith. “Having health insurance plays a major role in whether or not a woman has access to care providers who can monitor symptoms and act on those symptoms if necessary.”
The study authors were able to measure the improvement in ovarian cancer and treatment by using a difference-in-differences approach, which allows analysis using a comparator control group that is unaffected by the changes being evaluated. In this case, the investigators compared younger women with those ≥65 years of age, who would likely be on Medicare and uninfluenced by the passage of ACA.
In the United States, 22,000 women receive a diagnosis of ovarian cancer each year. More than 75% of those with early-stage ovarian cancer live 5 years or more; that percentage falls to less than 30% for those diagnosed at an advanced stage. As there is no screening test to detect ovarian cancer at an early stage, the cancer can often be present but undetected for years, due in part to the cancer’s tendency to present subtle symptoms. The coverage that the ACA afforded to an expanded number of Americans enabled women with the cancer to not only visit their doctors, but also report symptoms to their physicians, complete laboratory tests to confirm the presence of cancer, and subsequently receive treatment. The expanded coverage accessible through the ACA rendered early detection of the cancer increasingly possible.
By 2017, nearly 12.7 million individuals gained health coverage following the ACA’s 2010 implementation. Meanwhile, the proportion of uninsured Americans decreased from 16% in 2010 to less than 12% by 2016.
The investigators used data on stage at ovarian cancer diagnosis and time to treatment for women aged 21 to 64 and ≥65 who were diagnosed from 2004 to 2009 (pre-ACA; 35,842 patients) and 2011 to 2014 (post ACA; 37,145 patients).
Investigators examined the type of insurance women had and adjusted findings for race, rural demographics, neighborhood household income, education level, distance traveled for care, Census region, and practice setting for care. They also adjusted based on the Charlson comorbidity score, which predicts risk of death within 1 year of hospitalization for people with comorbid conditions.
The study was funded by a Johns Hopkins Department of Gynecology and Obstetrics Kelly Society Grant, and the investigators will expand their purview to include the years beyond 2014, to assess the impact of the ACA on early-stage diagnosis and treatment for women with gynecologic cancers.
Reference:
Smith AJ, Nickles Fader A. Impact of the Affordable Care Act on early-stage diagnosis and treatment for women with ovarian cancer.J Clin Oncol. 2019;37(suppl; abstr LBA5563).
PTCy Offers New Hope for Mismatched Stem Cell Transplants in Leukemia, MDS
April 13th 2024Jeff Auletta, MD, discussed how PTCy-based graft-vs-host disease prophylaxis offers a promising approach for expanding access to successful cell transplantation regardless of donor match or patient ethnicity.
Read More