Response to Checkpoint Inhibition in Urothelial Cancer May Be Affected by Autoimmune Events
The development of an immune-related adverse event was associated with improved patient response in an FDA analysis of patients with advanced urothelial cancer treated with a PD-1/PD-L1 inhibitor.
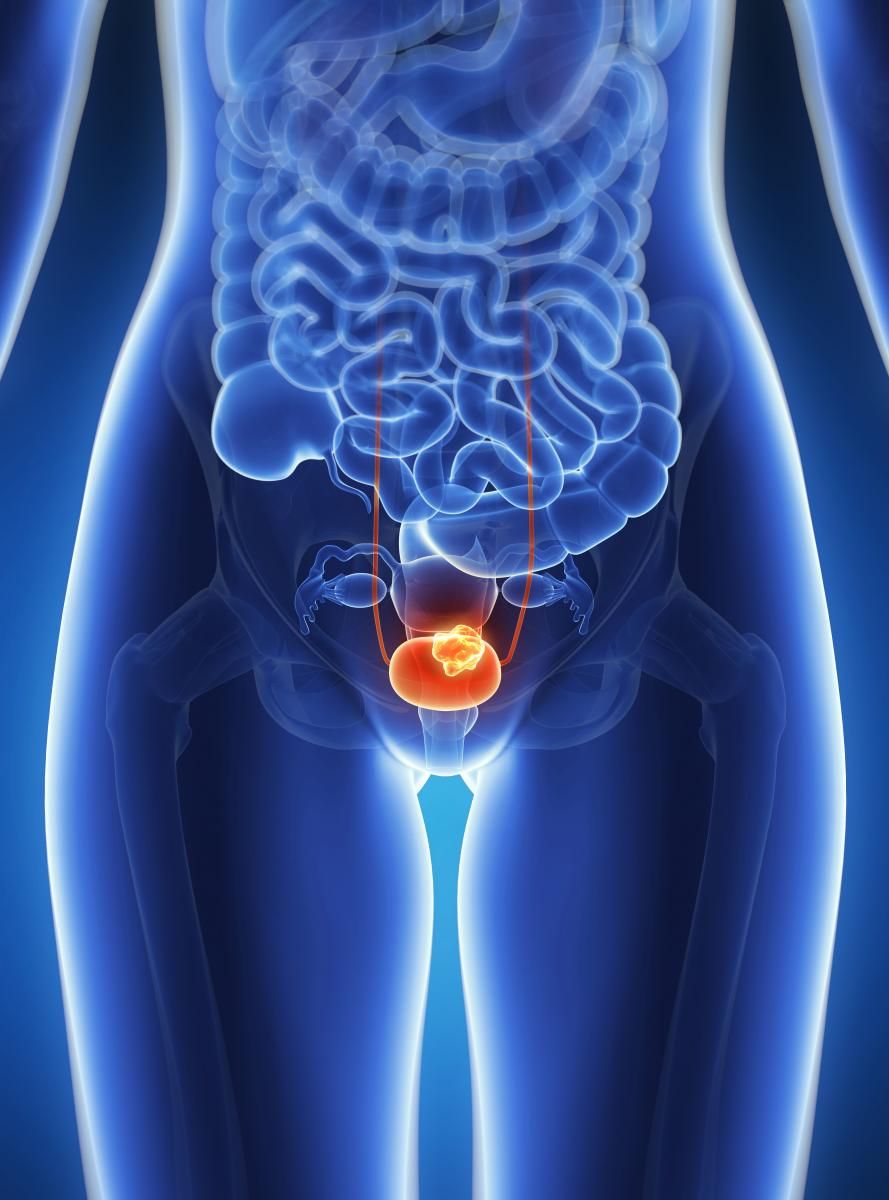
The development of an immune-related adverse event (AE) was associated with improved patient response in an FDA analysis of patients with advanced urothelial cancer treated with a PD-1/PD-L1 inhibitor. According to the analysis presented in a poster at the 2019 ASCO Annual Meeting, the patients who responded to treatment with an immune checkpoint inhibitor were more likely to have reported a related AE of special interest or an immune-mediated AE (imAE).
“In these 1747 patients with advanced urothelial cancer treated with a PD-1/PD-L1 inhibitor, there appeared to be a relationship between the development of an autoimmune event and improved patient outcome,” the study authors from the FDA wrote in their poster. “This relationship remained when adjusted for the duration of exposure.”
The FDA investigators reviewed the results of 1747 patients with metastatic or locally advanced urothelial cancer across 7 trials of antiPD-1/PD-L1 therapies. Five of these trials included patients who had received prior platinum-based therapy and the other 2 included patients who were ineligible to receive cisplatin.
Two of the studies each focused on pembrolizumab (Keytruda) and atezolizumab (Tecentriq), and the 3 others investigated avelumab (Bavencio), durvalumab (Imfinzi), and nivolumab (Opdivo). Six out of 7 trials were single-arm studies, and one of the pembrolizumab trials was a randomized study.
Most of the AEs of special interest focused on autoimmune events, but also included broader terms, such as diarrhea or rash, as defined by each study’s protocol. The study authors focused on AEs of special interest that were thought to be related to the study drug as per the investigator. All imAEs were defined as AEs of special interest that were treated with topical or systemic corticosteroids.
Related AEs of special interest were reported in 64% of the 351 patients who responded to PD-1/PD-L1 inhibitor treatment and in 34% of the 1396 nonresponding patients. Related imAEs were reported in 28% of the responding patients and in 12% of the nonresponding patients.
The study authors adjusted the rates according to the duration of exposure and found that the odds ratio of having a related AE of special interest was 5.38 (95% CI, 3.06-9.46) for responders versus nonresponders and was 3.77 (95% CI, 2.02-7.03) for having a related imAE.
Of note, 57% of patients who responded to checkpoint inhibition and had a related AE of special interest reported an AE prior to the documentation of their response. Other AEs of special interest also occurred after the documentation of a response.
An increase in overall survival was seen in patients with a related AE of special interest as compared with patients who did not have any related AE of special interest (HR, 0.45; 95% CI, 0.39-0.52).
Patients who responded to treatment appeared to have a similar duration of response whether they received a systemic corticosteroid or not for any reason (HR, 1.09; 95% CI, 0.70-1.69).
Reference:
Maher VE, Fernandes LL, Weinstock C, et al. An FDA analysis of the association between adverse events and outcome in patients with urothelial cancer receiving a programmed death protein 1 or programmed death ligand 1 (anti-PD-1/L1) antibody.J Clin Oncol.2019;37(suppl 15; abstr 4549). meetinglibrary.asco.org/record/172228/abstract.
Study Shows Desire for Bladder-Sparing Treatments in High-Risk NMIBC
April 2nd 2024In an interview with Targeted Oncology, Joseph M. Jacob, MD, discussed how bladder preservation is the top reason for refusal of radical cystectomy in the TAR-200 monotherapy cohort of the SunRISe-1 study.
Read More