Wang Discusses Treatment Options for Patients With Intermediate-Risk Mantle Cell Lymphoma
Michael L. Wang, MD, explains the biologic underpinnings of MCL as well as the treatment options for patients with MCL. The discussion is based on a case scenario of a patient with stage III intermediate-risk disease, and the factors that Wang would use when choosing the best treatment regimen for this patient.
Michael L. Wang, MD
Michael L. Wang, MD, a professor in the Department of Lymphoma and Myeloma at MD Anderson Cancer Center, explains the biologic underpinnings of mantle cell lymphoma (MCL) as well as the treatment options for patients with MCL. The discussion was framed around a case scenario of a patient with stage III intermediate-risk disease, and the factors that Wang would use when deciding on treatment for this patient.
TARGETED ONCOLOGY:Explain the disease background of MCL.
Wang:MCL is a rare subtype of B-cell lymphoma. In the United States, 1 million citizens live with lymphoma. Overall, lymphoma has 2 parts: Hodgkin lymphoma and non-Hodgkin lymphoma. Non-Hodgkin lymphoma includes T-cell lymphoma, [with a frequency of] about 5% to 10%, but the vast majority is B-cell lymphoma, which is about 85% to 90%. Within B-cell lymphoma, which is the most common type of lymphoma, there are many subtypes. Large cell lymphoma is most common, followed by follicular lymphoma and then marginal zone lymphoma. MCL is a rare subtype of B-cell lymphoma that is not yet curable, but much progress has been made in this eld. There are specific medicines approved by the FDA just for MCL.
MCL is driven by cyclin D1. With the 11;14 translocation, there’s also cyclin D1, which is supposed to drive the pathogenesis of MCL. And when there’s a translocation of this gene from the 11th chromosome on to the 14th chromosome, where there’s a heavy chain promoterheavy chain is around the most number of proteins, there is a lot of it in our body, so this promoter has a lot of work to do—it drives the B cell to make a lot of heavy chain antibodies. So, if any protein gene is placed after this promoter, it overdrives the protein expression. In this case, it happens under genetic environmental factors. The cyclin D1 gene is misplaced on the 14th chromosome, just after the heavy gene promoter. That’s overproduction of cyclin D1, which could drive the pathogenesis of MCL together with many factors on the molecular and cell pathway levels.
With morphologic variants, there’s a controversy, but most variants are nodular, morphologically diffuse, pleomorphic, and blastoid. Nodular has the slowest growth rate, and diffuse is a little faster. The slowest is indolent MCLthe nodular. Pleomorphic is very aggressive, and blastoid is the most aggressive. Sometimes, people think the slowest MCL is mantle zone lymphoma, as described by a hematopathologist from The University of Texas MD Anderson Cancer Center, but it’s not overly used.
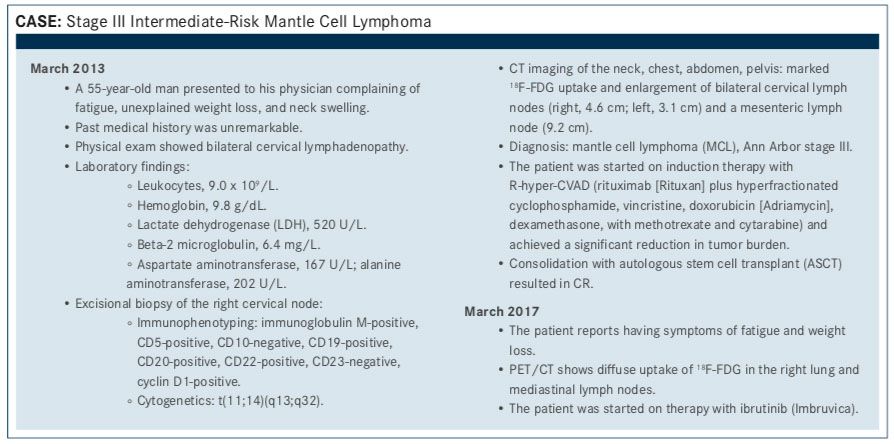
TARGETED ONCOLOGY:What is the prognosis for this patient?
Wang:The MIPI (Mantle Cell Lymphoma International Prognostic Index) score for this patient is over 6, and MIPI scores are often used in publications. When you publish something on MCL, you have to use the MIPI score, but not all doctors calculate a MIPI score before they give therapy. For example, this patient needs therapy because he has symptoms and a big tumor. You do not need a MIPI score to tell you that this patient needs immediate therapy.
This patient has a big tumor, tumors above and below the diaphragm, and is young. The regular therapiesR-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone) or BR (bendamustine [Treanda] plus rituximab)—are inadequate for this patient. This patient has to get intensive therapy.
If you’re very familiar with the therapy and natural history of MCL, you don’t need a MIPI score. But if you don’t treat it yearlyon average, community doctors in their entire oncological career treat 1 to 2 patients with MCL—please calculate the MIPI. The MIPI calculation is rather complicated if you do it manually, but there’s an online formula.
TARGETED ONCOLOGY:What are the choices for induction therapy for this patient?
Wang:According to the Nordic 2 clinical trial, the median survival was 12.5 years, so it was a great trial and people got to live for more than 12 years. However, chemotherapies are DNA breakers. They attack the tumor DNA, but at the same time, these intensive therapies also attack the normal, human DNA. Of the patients on the Nordic trial, 12% of them had another form of malignancy we call the secondary malignancies. We cannot use this therapy forever without improvement. At The University of Texas MD Anderson Cancer Center, we did a clinical trial, called the WINDOW-2 clinical trial, which used ibrutinib with rituximab to induce CR followed by 4 cycles of hyper-CVAD (hyperfractionated cyclophosphamide, vincristine, doxorubicin (Adriamycin), dexamethasone, with methotrexate and cytarabine) without stem cell transplantation (NCT02427620).
This therapy was presented at the 2016 American Society of Hematology (ASH) Annual Meeting, and the updated trial was presented in June at the 2017 International Malignant Lymphoma meeting. The overall response rate (ORR) was 100% before chemotherapy and the complete remission (CR) rate was 90% before chemotherapy, so we do not need a lot of chemotherapy to get long-term survival. Although I have to caution, the WINDOW-2 clinical trial follow-up time is still short. So, I wouldn’t say that these patients were treated in a standard-of-care way. But if this patient presented at MD Anderson, I would put him into the WINDOW clinical trial.
I think the most important therapy is the first therapy. Frontline therapy is the most important therapy in aggressive lymphoma, and this is especially true for MCL. If you mess up the frontline therapy, you could mess up a long-term remission. If you treat the patient with a good therapy, the patient can be therapy free for 10 years. But you shouldn’t treat a young patient, such as this case, with an inadequate therapy, such as R-CHOP for 6 cycles or BR. Those are only for elderly people who could not tolerate intensive therapy, such as stem cell transplantation.
Frontline therapy for a young, fit patient has to have intensity. Because the tumor is an icebergyou can see what’s above the water with scans, blood tests, and bone marrow examinations, but what is below the water is maybe even 70% to 90% of the tumor that you cannot see. If you use the super cial therapies—R-CHOP or BR—you shape what’s above the water, the scans become negative, and you think the patient is doing great. And shortly after, in a year or 2, the base grows very aggressively. They are no longer chemotherapy-sensitive.
TARGETED ONCOLOGY:Discuss the use of minimal residual disease (MRD) testing to monitor response.
Wang:People always said this is a very common idea: you treat the patient, and the scans or bone marrow biopsy, the common routine for receding criteria, have already yielded a CR. Then you check the MRD, either by flow cytometry or sequencing data, and you find there is disease left. This means you’d still find residual disease, which means you did not get rid of the root of the iceberg. MRD is underutilized. If you treat MCL, the quickest way to restage MCL is after 2 months.
However, our national guidelines do not allow you to do a PET scan within 60 days. It is not convenient to do scans every 2 weeks or every month. The patient’s body cannot take that amount of radiation. But if you are able to use the blood test, you can see MRD going down. It means your chemotherapy is working and you should continue. And if their MRD goes up, we need to change the chemotherapy. So, MRD can not only tell you the prognosis of the patient after nishing therapy, but it can also provide an opportunity to intervene in giving therapy.
MRD is also a technology for early detection. In the future, with MRD sophistication coupled with big data, we may be able to detect cancer before it forms a tumor, [meaning] you can use much less therapy to get rid of the MRD, so that patient will easily get into remission without a lot of toxicities. So, MRD is exciting.
TARGETED ONCOLOGY:What is the rationale for using ibrutinib versus rechallenge with R-hyper-CVAD or using another chemotherapy regimen?
Wang:I would predict the patient will relapse within 5 years because of his high MIPI score and the fact that his tumor was 9 cm in the abdomen. So, it does not surprise me that the patient relapsed roughly 4 years after initial therapy. Then the patient was treated with ibrutinib.
Ibrutinib is a small molecule targeting the Bruton’s tyrosine kinase (BTK), which is an important component of the B-cell receptor pathway, from the surface of the B cell to the nucleus of the B cell. BTK is in the cytosol part of that pathway, and once it’s blocked with ibrutinib or you knock the gene out, the cell dies. Ibrutinib was approved in November of 2013 by the FDA through a breakthrough mechanism based on the results of a phase II clinical trial that was not intentionally meant for FDA approval.1
It was unprecedented in ef cacy, with a 68% ORR and a CR rate over 20%. You may not think that this is impressive, but if you use ESHAP (etoposide, methylprednisolone, cytarabine [Ara-C], and cisplatin), you need to admit the patient to the hospital for therapy, the patient will lose their hair, and their blood count goes down. They need transfusions. They need to ght infections. And their response rate is about 65% to 70% [with ESHAP]. Now, we can achieve this without giving the patient all of these chemically toxic combinations. We do not have to use an intravenous catheter. We can just give the patient a pill once a day and achieve the same purpose. So, this was a milestone in the therapy of MCL.
TARGETED ONCOLOGY:How do you typically use ibrutinib in MCL?
Wang:Ibrutinib is given at 560 mg. The patient will take 4 capsules in the morning on an empty stomach. The most common side effects are fatigue, loose stools not qualifying for diarrhea, and sometimes a little petechiae. Like aspirin, there are very common bleeding issues, but nothing severe. If you do not use it with other blood thinners, such as warfarin, Xarelto (rivaroxaban), or aspirin, the bleeding is not very heavy, not very risky. However, you need to caution all patients who take ibrutinib: try not to fall, avoid contact sports, avoid riding a bicycle. In that clinical trial, about 4 patients had subdural hematoma, intracranial bleeding. They were also associated with trauma, such as a fall. So, avoid trauma and be aware that ibrutinib is a bleeder.
Ibrutinib can sometimes cause a rash, especially in young people. It’s not an allergy. If you stop the drug for a few days and use a Medrol Dosepak, it goes away almost all the time. Don’t be afraid of the rash, but be aware of the severe bleeding risk. The most dreaded side effect is atrial fibrillation. For about 6% of people, especially elderly people who are above 70 years old and have a history of long-term hypertension, who have a history of a cardiac disease, ibrutinib could induce atrial fibrillation.
When the patient has atrial fibrillation, I would avoid using ibrutinib. This is not the general guideline you would hear, but I become very cautious when the patient has atrial fibrillation. I often ask the patient to have a nodal ablation from the cardiologist. Nodal ablation is not a regular indication for this kind of atrial fibrillation, but oncology is changing the protocol for cardiology. Many cardiologists are collaborating with us to put
the patient into normal sinus through nodal ablation so we can resume ibrutinib.
A good CR occurs in 20%, according to the old Cheson criteria. If you use the new, updated Lugano criteria, the CR rate will be much higher. It will be in about 30% to 40%, to the best of my knowledge. CR does happen if you use PET scan. With PET scan negativity, we call that complete metabolic response. The response is about 70%, and if you are able to steer the patient away from those toxicities, the patient could stay on the drug for as long as 5 years.
TARGETED ONCOLOGY:What are some of the up-and-coming treatment options for patients with MCL?
Wang:There’s a newer BTK inhibitor called ACP-196 (acalabrutinib; Calquence) that has a different toxicity profile [than ibrutinib].
There’s another trial of venetoclax (Venclexta), a BCL-2 inhibitor. In a clinical trial published in the Journal of Clinical Oncology this year by Matthew Davids, MD, MMSc, from Harvard, the response rate was 75%.2 So, this is an even better response, but it needs to be validated in a clinical trial with more patients. Venetoclax has been approved for chronic lymphocytic leukemia, and I’m sure in the future it could be approved for MCL.
All of those are small molecule pathway interrogators. Each drug usually works for about 12 to 24 months, and after that, the patient inevitably develops either intolerance or resistance. So, those options are not cures. Immunotherapy is coming and could provide longer remissions. There are very exciting clinical trials for CAR (chimeric antigen receptor) T cells. There’s one dedicated FDA pivotal trial, called the ZUMA-2 clinical trial, from Kite Pharma, with very promising results so far.
References:
- Wang ML, Rule S, Martin P, et al. Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2013;369(6):507-516. doi: 10.1056/ NEJMoa1306220.
- Davids MS, Roberts AW, Seymour JF, et al. Phase I first-2. in-human study of venetoclax in patients with relapsed or refractory non-Hodgkin lymphoma. J Clin Oncol. 2017;35(8):826-833. doi: 10.1200/JCO.2016.70.4320.
Biomarker Testing Paves the Way for Better Targeted Therapies in NSCLC
April 16th 2024At a live virtual event, Edward S. Kim, MD, MBA, discussed the evolving landscape of biomarker testing before making treatment decisions for patients with early-stage non–small cell lung cancer (NSCLC).
Read More
Creating Solutions for a 'Continual State of Transition' in Cancer Care
April 15th 2024In a Peers & Perspectives in Oncology feature article, we focus on the importance of the transition-of-care process for patients with cancer as they move from the inpatient to outpatient setting, as well as between lines of therapy with comments from Marc J. Braunstein, MD, PhD, and Michael Shusterman, MD.
Read More