Optimizing FLT3 Inhibitor Monotherapy in Acute Myeloid Leukemia
Acute myeloid leukemia (AML) therapy is guided mainly by cytogenetic profile, such as chromosomal duplication or deletion, and molecular mutations. <em>FLT3</em> mutations are the most common genetic abnormalities detected in patients with AML and are usually associated with a high relapse rate and short overall survival. Given the dismal outcomes in patients with <em>FLT3</em>-mutant AML, a great effort has been underway over the last several years to develop clinically effective FLT3 inhibitors.
Amro Elshoury, MBCHB
Abstract
Acute myeloid leukemia (AML) therapy is guided mainly by cytogenetic profile, such as chromosomal duplication or deletion, and molecular mutations.FLT3mutations are the most common genetic abnormalities detected in patients with AML and are usually associated with a high relapse rate and short overall survival. Given the dismal outcomes in patients withFLT3-mutant AML, a great effort has been underway over the last several years to develop clinically effective FLT3 inhibitors. In May 2017, the FLT3 inhibitor midostaurin was approved for the upfront treatment of newly diagnosed patients withFLT3-mutant AML in combination with cytarabine-based induction and consolidation therapy. Currently, several other tyrosine kinase inhibitors are being evaluated in patients withFLT3-mutated AML, either as a monotherapy or in combination with systemic chemotherapy. This review aims to explore the current and future directions of FLT3 inhibitor monotherapy in various clinical settings forFLT3-mutant AML, including frontline and relapsed disease as well as maintenance following allogeneic stem cell transplantation.
Clinical Significance of Aberrant FLT3 Signaling in Acute Myeloid Leukemia
Acute myeloid leukemia (AML) therapy is guided mainly by the molecular and cytogenetic profile.FLT3mutations are the most common genetic abnormalities detected in patients with AML (30%) and are encoded by a gene located on chromosome 13q12.1There are 2 main types ofFLT3mutations.2The first type is composed of internal tandem duplications (FLT3-ITD mutations) in or near the juxtamembrane domain of the receptor, which occurs predominantly in cytogenetically normal AML. The second type is composed of missense point mutations resulting in substitutions of single amino acids, mostly aspartic acid 835, in the activation loop of the tyrosine kinase domain (FLT3-TKD mutations). Both types of mutations lead to constitutive activation of FLT3 kinase in a ligandindependent manner with subsequent activation of multiple downstream signaling pathways, including STATs, MAP, and PI3K/AKT kinase pathways; this leads to uncontrolled cell proliferation and survival.3Although, patients withFLT3-mutant AML can achieve remission with standard induction chemotherapy in a frequency comparable toFLT3-wild type AML, responses are usually transient with a high relapse rate and shorter overall survival (OS). Patients withFLT3-mutant AML with a high allelic burden are an exception, as they are usually refractory to standard induction chemotherapy.4
Given the dismal outcomes in patients withFLT3-mutant AML, a great effort has been underway over the last several years to develop clinically effective FLT3 inhibitors. In May 2017, the FLT3 inhibitor midostaurin was approved for the upfront treatment of newly diagnosed patients withFLT3mutations in combination with cytarabine-based induction and consolidation therapy. Currently, several other tyrosine kinase inhibitors (TKIs) are being evaluated in patients withFLT3-mutated AML, either as a monotherapy or in combination with systemic chemotherapy. This review aims to explore the current and future directions of FLT3-inhibitor monotherapy in various clinical settings forFLT3-mutant AML, including frontline and relapsed disease as well as maintenance following allogeneic stem cell transplantation.
Overview of FLT3 Inhibitors
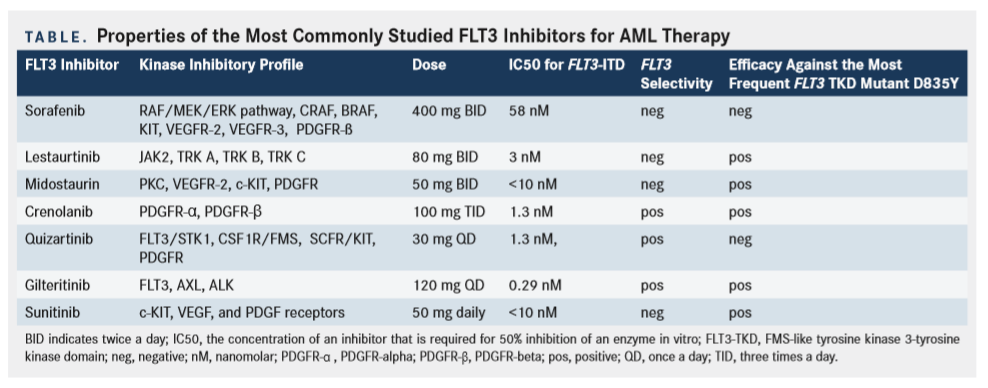
First-generation FLT3 inhibitors are broad-spectrum multikinase inhibitors that were not originally developed to selectively target FLT3 exclusively, but to target various other kinases such as c-KIT, JAK2, PDGFR-B and VEGFR.5This group includes sorafenib, sunitinib, lestaurtinib, and midostaurin. In contrast, second-generation FLT3 inhibitors were primarily developed to specifically block FLT3 as their main target. Therefore, they are potent, selective, and ideally capable of maintaining substantial and sustained FLT3 inhibition at clinically tolerable doses. Second-generation FLT3 inhibitors include quizartinib, crenolanib, and gilteritinib. A summary comparing the properties of the FLT3 inhibitors with recent clinical data are provided in theTable.
First-Generation FLT3 Inhibitors
Sunitinib
Sunitinib (previously known as SU11248) is an oral multikinase inhibitor capable of inhibiting multiple important pathways responsible for leukemogenesis. In addition to inhibitingFLT3, sunitinib also inhibits c-KIT, VEGF, and PDGF receptors.6In a phase I study, 15 patients with refractory AML or de novo AML not eligible for conventional induction chemotherapy received sunitinib 50 mg daily for 4-week cycles followed by either a 1- or a 2-week rest period.7All patients withFLT3mutations (2 patients withFLT3-ITD and 2 patients withFLT3-D835) had morphologic or partial responses (PRs).FLT3mutation was no longer detected in 2 patients after 4 weeks of therapy. On the other hand, only 2 of the 10 evaluable patients withFLT3wild-type AML had responses. Of note, although the durations of clinical responses were short-lived regardless ofFLT3mutational status, patients withFLT3-mutant AML appeared to have relatively earlier and longer disease responses.
Lestaurtinib
Lestaurtinib (formerly known as CEP-701), another first-generation FLT3 inhibitor, was initially evaluated for the management of prostate cancer due to its activity against neurotrophin-specific TRK receptors.8Lestaurtinib subsequently demonstrated antileukemic activity against FLT3-mutated AML in preclinical and phase I and II studies. In a phase I/II trial, 14 heavily pretreated patients with relapsed/refractory (r/r)FLT3-mutant AML received lestaurtinib at an initial dose of 60 mg orally twice daily.9Five patients (36%) had evidence of clinical response: 1 patient had a decrease in bone marrow blasts to less than 5%, and 4 patients had significant reductions in peripheral blood blast counts. Unfortunately, all clinical responses were short-lived, ranging from 2 weeks to 3 months. Lestaurtinib monotherapy was also evaluated as an upfront therapy in patients with AML unfit for standard induction chemotherapy.10In a phase II study, 27 patients with AML (5 patients withFLT3mutations and 22 patients withFLT3wild-type) older than 60 years who were considered unfit for standard induction chemotherapy received lestaurtinib at an initial dose of 60 mg twice daily. The dose was then escalated to 80 mg twice daily, irrespective ofFLT3mutation status. Eight patients (3 with mutantFLT3and 5 with wild-typeFLT3) had transient reductions in bone marrow and peripheral-blood blasts. However, median time to progression was only 25 days. These discouraging results were ascribed in part to the failure of this agent to achieve robust and sustained in vivo FLT3 inhibition. This might be due to the fact that lestaurtinib is highly bound to plasma protein, specifically alpha-1-acid glycoprotein. This agent is currently no longer in clinical development.
Sorafenib
Sorafenib is a broad-spectrum multikinase inhibitor approved for the treatment of renal cell carcinoma, hepatocellular carcinoma, and thyroid carcinoma. Its antineoplastic activity is attributed to its ability to inhibit various tyrosine kinases involved in tumorigenesis, including BRAF, c-KIT, FLT3, RET, VEGFR-1, VEGFR-2, VEGFR-3 and PDGFR-β. Despite having a long mean elimination half-life of approximately 25 to 48 hours, sorafenib is dosed twice daily with a maximum daily dose of 800 mg. Sorafenib is metabolized through the cytochrome P450 system, primarily through CYP3A4 as well as glucuronidation by UGT1A9. This drug metabolism pathway makes sorafenib susceptible to numerous drugdrug interactions. Elimination of sorafenib occurs primarily through the feces (77%) with minor excretion through the urine (19%). Based on its pharmacokinetics, no dose adjustments are needed for renal or hepatic impairment.
Due to its ability to target FLT3, sorafenib monotherapy was first studied in patients with r/r AML. Although these early studies demonstrated clinical benefit as reflected by morphologic remissions, these responses were not durable, and deep molecular and cytogenetic responses were not obtained.11-15From a pharmacodynamic perspective, this may be due to the fact that first-generation FLT3 inhibitors such as sorafenib are not highly selective or specific for FLT3. Therefore, only a fraction of patients are able to achieve a complete and sustained FLT3 inhibition with this agent, thereby limiting its clinical use as monotherapy for a known aggressive malignancy.16
Sorafenib has demonstrated promising data as maintenance therapy to further improve outcomes of allogeneic stem cell transplant (alloSCT) for patients withFLT3-mutant AML. Despite the clinical benefit of alloSCT for these patients, there remains a significant risk of disease recurrence after transplantation due to residual disease.17-19In a retrospective study of 26 patients withFLT3-ITDmutation AML (of whom 7 also received sorafenib prior to alloSCT), posttransplant sorafenib maintenance in the setting of morphologic complete remission (CR) was associated with an improved 2-year OS (81% vs 62%; P = .029), improved 2-year progression-free survival (PFS) (82% vs 53%; P = .0081) and lower 2-year cumulative incidence of relapse (8.2% vs 37.7%; P = .0077), compared with patients not receiving sorafenib.20Sorafenib has also been utilized in the posttransplant setting for treatment of relapsedFLT3-mutant disease. In this setting, sorafenib monotherapy theoretically could synergize with the allo-immune effects of the transplant to enhance antileukemic effects.21-23However, to date, while clinical benefit of sorafenib monotherapy in this setting has been seen, responses are once again not durable, with emergence of resistant AML. Of note, prolonged sorafenib monotherapy has been shown to lead to the development of AML cells containing theFLT3TKD mutation, conferring drug resistance. Thus, based on the current available literature, sorafenib monotherapy following alloSCT should ideally be used in the maintenance setting to prevent further disease recurrence rather than to treat overt disease relapse.
Midostaurin
As noted above, the first-generation FLT3 inhibitor midostaurin (formerly known as PKC412) was recently approved in the United States for treatment of newly diagnosedFLT3-mutant AML in combination with standard induction and consolidation therapy consisting of cytarabine plus daunorubicin. Midostaurin is a multitargeted TKI originally developed as a protein kinase C inhibitor, which was subsequently found to potently inhibit other class III tyrosine kinase receptors including FLT3, VEGFR-2, c-KIT, and PDGFR-alpha.24A phase II study employing midostaurin in patients withFLT3-mutant AML demonstrated a well-tolerated dose with encouraging clinical response.16Twenty patients with relapsedFLT3-mutant AML or high-grade myelodysplastic syndrome (MDS) received midostaurin at a dose of 75 mg 3 times daily by mouth. Fourteen patients (70%) had a 50% reduction in peripheral blasts, and 7 patients (35%) experienced a greater than 2-log reduction in peripheral blast counts for more than 4 weeks. These encouraging results led to further studies of midostaurin in patients with AML with both wild-type and mutatedFLT3. A phase IIb study of midostaurin monotherapy was performed in 95 patients with AML or high-risk MDS. Two-thirds had wild-typeFLT3disease (n = 60) and one-third (n = 35) had mutatedFLT3(n = 35) disease. Patients were randomized to receive midostaurin at a dose of either 50 or 100 mg twice daily.25Midostaurin monotherapy induced significant but transient decreases in peripheral and bone marrow blasts. Selectively enhanced responses were reported among those patients whose disease harboredFLT3mutations, with 71% experiencing blast reduction as compared with 42% of patients with wild-typeFLT3AML. The failure of midostaurin monotherapy to maintain durable clinical responses provided the rationale for eventually combining midostaurin with cytotoxic chemotherapy in the upfront setting to further improve outcomes.26
Second-Generation FLT3 Inhibitors
Second-generation FLT3 inhibitors were designed specifically to exert clinical activity in patients withFLT3-mutant AML. As compared with the firstgeneration inhibitors, these agents exhibit far more selectivity, specificity, and potency for FLT3 kinases, with limited inhibition of other off-target tyrosine kinases. This class of inhibitors includes quizartinib, crenolanib, and gilteritinib. As anticipated, these agents have consistently resulted in improved antileukemic activity in patients withFLT3-mutant AML, as reflected by higher response rates and, most importantly, evidence of prolonged diseasefree survival in the r/r setting. However, important distinctions exist among these agents.
Quizartinib
Quizartinib (previously called AC220) is among the most potent second-generation FLT3 inhibitors available.27Quizartinib is also highly selective and can completely inhibit FLT3 in vivo at clinically achievable doses. In a phase I study, 76 patients with r/r AML received quizartinib, irrespective of theirFLT3mutational status.28The objective response rate (ORR) was 30%. Compared with patients who are FLT3-ITD negative, patients who areFLT3-ITDpositive had a higher ORR (53% vs 14%). These encouraging results led to another phase II study wherein 76 patients (≥60 years old) with r/rFLT3-ITDmutant AML were randomized to receive quizartinib at a dose of 30 or 60 mg/day orally during continuous 28-day cycles. The composite CR rate in both cohorts was 47%. Adverse effects (AEs) included diarrhea (18%), neutropenic fevers (16%), and QT prolongation (15%). Resistance to quizartinib monotherapy inFLT3-ITD patients again appears to occur in large part due to the evolution of resistance-conferring point mutations inFLT3-TKD. Paired pretreatment and relapse bone marrow samples from 8 patients withFLT3-ITDmutant AML, all of whom initially achieved CR to quizartinib monotherapy and then subsequently relapsed, consistently revealed secondary TKD point mutations at the time of relapse that were not present in pretreatment samples.5
Crenolanib
Crenolanib is a type I TKI that binds mutantFLT3kinases in their active and inactive conformation. This agent has demonstrated activity against bothFLT3-ITD andFLT3-TKD mutations, including D835- and F691-activating mutations.29As a secondgeneration FLT3 inhibitor, crenolanib is highly selective for FLT3 (Kd0.74 nM) and lacks significant binding to cKIT (Kd78 nM), which may reduce the potential for myelosuppression. Crenolanib also has a unique pharmacokinetic profile with rapid absorption within 1.5 to 2 hours, maximal FLT3 inhibition within 2 to 3 hours, and, more importantly, a steadystate pharmokinetic profile and a short half-life
(6 to 8 hours). In contrast to midostaurin, these properties enable chronic long-term dosing of crenolanib without drug accumulation. Because crenolanib is eliminated within 2 days of stopping treatment, this agent is scheduled on a thrice-daily dosing regimen to maintain optimal drug levels. These favorable drug pharmacokinetics facilitate dosing crenolanib on a schedule that delivers sustained FLT3 inhibition while maintaining tolerability and minimizing drugdrug interactions.
In an open-label single-center phase II study of crenolanib in heavily pretreated patients with r/rFLT3-mutant AML, 38 patients received crenolinib monotherapy at a dose of 200 mg/m2/day 3 times a day orally continuously in 28-day cycles.30Crenolanib was well tolerated with no drug-related toxicity or deaths. The most common grade 3 AEs were abdominal pain and nausea. The ORR was a striking 47%. Compared with patients who received prior FLT3 inhibitor therapy, FLT3 inhibitornaïve patients had significantly longer median event-free survival (13 vs 7 weeks; P <.001) and OS (55 vs 13 weeks; P = .03).
These results have led to a phase II trial wherein crenolanib was used in combination with standard 7 + 3 induction and histone deacetylase consolidation chemotherapy in newly diagnosed patients withFLT3-mutant AML.31Moreover, a phase III study (ARO-021) randomizing newly diagnosed patients withFLT3-mutated AML to either crenolanib or midostaurin in combination induction and consolidation therapy is planned to start later this year.
Gilteritinib
Gilteritinib (formerly known as ASP2215) is a potent, selective, and sustained second-generation FLT3 inhibitor that also targets AXL. Preclinical studies have shown that the receptor tyrosine kinase, AXL, is important for constitutive FLT3 phosphorylation and activity in FLT3-ITDmutant AML.32Inhibition of AXL suppresses the growth of human FLT3-ITDmutant AML in vivo, making AXL a potential therapeutic target of much interest in patients withFLT3-mutant AML. AXL has also been implicated in modulating resistance to FLT3-targeted therapy.33Because of its ability to targetFLT-ITD and -TKD mutations as well as the secondary signaling AXL pathway, gilteritinib has translated into significant efficacy when used as a single agent for r/rFLT3-mutant AML.34Perl and colleagues recently published the results of a phase I/II study of 252 adults 18 years or older with r/r AML who received gilteritinib once daily at escalating doses according to a 3 + 3 design. Seventy-six percent had disease harboring FLT3 mutationsof these, 85% wereITDmutations, 7% wereTKDmutations, and 8% had bothITDandTKDmutations. Overall, gilteritinib was well tolerated with a maximum tolerated dose of 300 mg/day. Most common grade 3/4 AEs irrespective of relationship to treatment were febrile neutropenia (39%), anemia (24%), thrombocytopenia (13%), sepsis (11%), and pneumonia (11%). Common treatment-related AEs included diarrhea (37%), anemia (34%), fatigue (33%), and transaminitis (increased alanine aminotransferase in 19% and aspartate aminotransferase in 26%). By pharmacodynamic assays, at least 90% inhibition of FLT3 phosphorylation in AML cells was seen by day 8 in most patients receiving a daily dose of 80 mg or higher. Also, of note, there was an exposure-related increased inhibition of FLT3 phosphorylation with increasing plasma concentrations of gilteritinib. Based on these clinical and pharmacodynamic findings, the starting dose of gilteritinib for future studies was established to be 120 mg once daily. ORR was 40% (100 out of 249 evaluable patients), with 8% complete response (CR), 22% incomplete CR (4% with incomplete platelet recovery and 18% with incomplete hematological recovery), and 10% partial response. At doses of gilteritinib of 80 mg or higher, the ORR exceeded 50%. In conclusion, gilteritinib has a favorable safety profile and significant efficacy as a single agent for r/rFLT3-mutant AML. Use of gilteritinib, a highly selective and potent inhibitor, as a single agent for r/r disease may have significant advantages as a novel therapeutic agent due to the fact that relapsedFLT3-mutant AML is usually a monoclonal disease.
Conclusions
The approval of midostaurin as the first FLT3 TKI for treatment of AML has ushered in a new era in targeted therapeutics for this disease. However, unlike BCR-ABL inhibitors for chronic myeloid leukemia, the clinical development of FLT3 TKIs forFLT3-mutant AML has been highly challenging. Responses to FLT3 inhibitor monotherapy vary depending on the type ofFLT3mutations as well as on the specific drug. Differences in the spectrum of kinase inhibition, as well as the potency and sustainability of FLT3 inhibition, can significantly influence clinical activity. In general, FLT3 inhibitor monotherapy appears to be most effective in minimal residual disease states (such as following allogeneic stem cell transplantation) and for r/r AML characterized by high clonal FLT3-mutant disease burden. As suggested by the recent designation of gilteritinib as a breakthrough therapy, monotherapy with highly potent and selective FLT3 inhibitors may be most beneficial in patients with r/rFLT3-mutant disease. However, many perils remain. Although complete remissions and prolonged disease-free survival can be achieved with single-agent FLT3 inhibition, many patients will eventually succumb to AML characterized byFLT3wild-type or therapy-resistant TKD mutations. Future prospective studies directly comparing the efficacy of different FLT3 inhibitors in various clinical scenarios for the treatment ofFLT3-mutant AML are needed.
Conflict of interest: The authors declare no conflict of interest.
Author contribution: All authors participated in writing the paper, and they reviewed and approved the final manuscript.
Acknowledgment: This work was supported by Roswell Park Cancer Institute and National Cancer Institute (NCI) grant P30CA016056. EW is also supported by the RPCI Alliance Foundation (Jacquie Hirsch Leukemia Research Fund).
References
- Carow CE, Kim E, Hawkins AL, et al. Localization of the human stem cell tyrosine kinase-1 gene (FLT3) to 13q12-->q13.Cytogenet Cell Genet.1995;70(3-4):255-257.
- Kelly LM, Liu Q, Kutok JL, et al. FLT3 internal tandem duplication mutations associated with human acute myeloid leukemias induce myeloproliferative disease in a murine bone marrow transplant model.Blood.2002;99(1):310-318.
- Hayakawa F, Towatari M, Kiyoi H, et al. Tandem-duplicated Flt3 constitutively activates STAT5 and MAP kinase and introduces autonomous cell growth in IL-3dependent cell lines.Oncogene.2000;19(5):624-631.
- Whitman SP, Archer KJ, Feng L, et al. Absence of the wild-type allele predicts poor prognosis in adult de novo acute myeloid leukemia with normal cytogenetics and the internal tandem duplication of FLT3: a cancer and leukemia group B study.Cancer Res.2001;61(19):7233-7239.
- Nguyen B, Williams AB, Young DJ, et al. FLT3 activating mutations display differential sensitivity to multiple tyrosine kinase inhibitors.Oncotarget.2017;8(7):10931-10944. doi: 10.18632/oncotarget.14539.
- O’Farrell AM, Abrams TJ, Yuen HA, et al. SU11248 is a novel FLT3 tyrosine kinase inhibitor with potent activity in vitro and in vivo.Blood.2003;101(9):3597-3605.
- Fiedler W, Serve H, Döhner H, et al. A phase 1 study of SU11248 in the treatment of patients with refractory or resistant acute myeloid leukemia (AML) or not amenable to conventional therapy for the disease.Blood. 2005;105(3):986-993.
- George DJ, Dionne CA, Jani J, et al. Sustained in vivo regression of Dunning H rat prostate cancers treated with combinations of androgen ablation and Trk tyrosine kinase inhibitors, CEP-751 (KT-6587) or CEP-701 (KT-5555).Cancer Res. 1999;59(10):2395-2401.
- Smith BD, Levis M, Beran M, et al. Single-agent CEP-701, a novel FLT3 inhibitor, shows biologic and clinical activity in patients with relapsed or refractory acute myeloid leukemia.Blood. 2004;103(10):3669-3676.
- Knapper S, Burnett AK, Littlewood T, et al. A phase 2 trial of the FLT3 inhibitor lestaurtinib (CEP701) as first-line treatment for older patients with acute myeloid leukemia not considered fit for intensive chemotherapy.Blood. 2006;108(10):3262-3270.
- Schroeder T, Zohren F, Saure C, et al. Sorafenib treatment in 13 patients with acute myeloid leukemia and activating FLT3 mutations in combination with chemotherapy or as monotherapy.Acta Haematol. 2010;124(3):153-159. doi: 10.1159/000320173.
- Röllig C, Brandts C, Shaid S, et al. Survey and analysis of the efficacy and prescription pattern of sorafenib in patients with acute myeloid leukemia.Leuk Lymphoma. 2012;53(6):1062-1067. doi: 10.3109/10428194.2011.637210.
- Pratz KW, Cho E, Levis MJ, et al. A pharmacodynamic study of sorafenib in patients with relapsed and refractory acute leukemias.Leukemia. 2010;24(8):1437-1444. doi: 10.1038/leu.2010.132.
- Borthakur G, Kantarjian H, Ravandi F, et al. Phase I study of sorafenib in patients with refractory or relapsed acute leukemias.Haematologica. 2011;96(1):62-68. doi: 10.3324/haematol.2010.030452.
- Fontanelli G, Rocco M, Caracciolo F, et al. Sorafenib as monotherapy or in association with cytarabine and clofarabine for the treatment of relapsed/ refractory FLT3 ITD-positive advanced acute myeloid leukemia.Clin Lymphoma Myeloma Leuk. 2014;14(1):e13-e17. doi: 10.1016/j.clml.2013.08.005.
- Stone RM, DeAngelo DJ, Klimek V, et al. Patients with acute myeloid leukemia and an activating mutation in FLT3 respond to a small-molecule FLT3 tyrosine kinase inhibitor, PKC412.Blood. 2005;105(1):54-60.
- Antar A, Kharfan-Dabaja MA, Mahfouz R, Bazarbachi A. Sorafenib maintenance appears safe and improves clinical outcomes in FLT3-ITD acute myeloid leukemia after allogeneic hematopoietic cell transplantation.Clin Lymphoma Myeloma Leuk. 2015;15(5):298-302. doi: 10.1016/j.clml.2014.12.005.
- Battipaglia G, Ruggeri A, Massoud R, et al. Efficacy and feasibility of sorafenib as a maintenance agent after allogeneic hematopoietic stem cell transplantation for Fms-like tyrosine kinase 3-mutated acute myeloid leukemia.Cancer. 2017;123(15):2867-2874. doi: 10.1002/cncr.30680.
- Chen YB, Li S, Lane AA, et al. Phase I trial of maintenance sorafenib after allogeneic hematopoietic stem cell transplantation for fms-like tyrosine kinase 3 internal tandem duplication acute myeloid leukemia.Biol Blood Marrow Transplant. 2014;20(12):2042-2048. doi: 10.1016/j.bbmt.2014.09.007.
- Brunner AM, Li S, Fathi AT, et al. Haematopoietic cell transplantation with and without sorafenib maintenance for patients with FLT3-ITD acute myeloid leukaemia in first complete remission.Br J Haematol. 2016;175(3):496-504. doi: 10.1111/bjh.14260.
- Metzelder S, Wang Y, Wollmer E, et al. Compassionate use of sorafenib in FLT3-ITDpositive acute myeloid leukemia: sustained regression before and after allogeneic stem cell transplantation.Blood. 2009;113(26):6567-6571. doi: 10.1182/blood-2009-03-208298.
- Metzelder SK, Schroeder T, Finck A, et al. High activity of sorafenib in FLT3-ITDpositive acute myeloid leukemia synergizes with allo-immune effects to induce sustained responses.Leukemia. 2012;26(11):2353-2359. doi: 10.1038/leu.2012.105.
- Sharma M, Ravandi F, Bayraktar UD, et al. Treatment of FLT3-ITD-positive acute myeloid leukemia relapsing after allogeneic stem cell transplantation with sorafenib.Biol Blood Marrow Transplant. 2011;17(12):1874-1877. doi: 10.1016/j.bbmt.2011.07.011.
- Propper DJ, McDonald AC, Man A, et al. Phase I and pharmacokinetic study of PKC412, an inhibitor of protein kinase C.J Clin Oncol. 2001;19(5):1485-1492.
- Fischer T, Stone RM, Deangelo DJ, et al. Phase IIB trial of oral midostaurin (PKC412), the FMS-like tyrosine kinase 3 receptor (FLT3) and multi-targeted kinase inhibitor, in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome with either wild-type or mutated FLT3. JClin Oncol. 2010;28(28):4339-4345. doi: 10.1200/JCO.2010.28.9678.
- Stone RM, Mandrekar SJ, Sanford BL, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation.N Engl J Med.2017;377(5):454464. doi: 10.1056/NEJMoa1614359.
- Zarrinkar PP, Gunawardane RN, Cramer MD, et al. AC220 is a uniquely potent and selective inhibitor of FLT3 for the treatment of acute myeloid leukemia (AML).Blood. 2009;114(14):2984-2992. doi: 10.1182/blood-2009-05-222034.
- Cortes JE, Kantarjian H, Foran JM, et al. Phase I study of quizartinib administered daily to patients with relapsed or refractory acute myeloid leukemia irrespective of FMS-like tyrosine kinase 3-internal tandem duplication status.J Clin Oncol. 2013;31(29):3681-3687. doi: 10.1200/JCO.2013.48.8783.
- Fathi AT. Emergence of crenolanib for FLT3-mutant AML.Blood. 2013;122(22):3547-3548. doi: 10.1182/blood-2013-10-528992.
- Randhawa JK, Kantarjian HM, Borthakur G, et al. Results of a phase II study of crenolanib in relapsed/refractory acute myeloid leukemia patients (pts) with activating FLT3 mutations results of a phase II study of crenolanib in relapsed/ refractory acute myeloid leukemia patients (pts) with activating FLT3 mutations.Blood. 2014;124(21):389.
- Wang ES, Stone RM, Tallman MS, et al. Crenolanib, a type I FLT3 TKI, can be safely combined with cytarabine and anthracycline induction chemotherapy and results in high response rates in patients with newly diagnosed FLT3 mutant acute myeloid leukemia (AML).Blood. 2016;128(22):1071.
- Park IK, Mishra A, Chandler J, et al. Inhibition of the receptor tyrosine kinase Axl impedes activation of the FLT3 internal tandem duplication in human acute myeloid leukemia: implications for Axl as a potential therapeutic target.Blood. 2013;121(11):2064-2073. doi: 10.1182/blood-2012-07-444018.
- Park IK, Mundy-Bosse B, Whitman SP, et al. Receptor tyrosine kinase Axl is required for resistance of leukemic cells to FLT3-targeted therapy in acute myeloid leukemia.Leukemia. 2015;29(12):2382-2389. doi: 10.1038/leu.2015.147.
- Perl AE, Altman JK, Cortes J, et al. Selective inhibition of FLT3 by gilteritinib in relapsed or refractory acute myeloid leukaemia: a multicentre, first-in-human, open-label, phase 1-2 study.Lancet Oncol. 2017;18(8):1061-1075. doi: 10.1016/ S1470-2045(17)30416-3.

Peers Discuss Role of Pola-R-CHP vs R-CHOP in Newly Diagnosed DLBCL
April 19th 2024During a Case-Based Roundtable® event, Haifaa Abdulhaq, MD discussed with participants whether the POLARIX trial influences their choice to use the pola-R-CHP as opposed to R-CHOP regimen for patients with newly diagnosed diffuse large B-cell lymphoma.
Read More
Powell Reviews Updated IO/TKI Data and AE Management in Endometrial Cancer
April 18th 2024During a Case-Based Roundtable® event, Matthew A. Powell, MD, discussed the case of a patient with advanced endometrial cancer treated with lenvatinib plus pembrolizumab who experienced grade 2 treatment-related hypertension.
Read More
Savona Discusses First-Line JAK Inhibition for Patients With Myelofibrosis at Risk of Anemia
April 17th 2024During a Case-Based Roundtable® event, Michael Savona, MD, and participants discussed the case of a patient with myelofibrosis and moderate anemia receiving JAK inhibitor therapy.
Read More
Biomarker Testing Paves the Way for Better Targeted Therapies in NSCLC
April 16th 2024At a live virtual event, Edward S. Kim, MD, MBA, discussed the evolving landscape of biomarker testing before making treatment decisions for patients with early-stage non–small cell lung cancer (NSCLC).
Read More