Early Study Shows Promise for Novel BET Inhibitor in Progressive Lymphomas
A novel bromodomain and extra terminal protein inhibitor demonstrated promising early activity and a manageable safety profile in the treatment of patients with relapsed or refractory lymphoma in the results of a first-in-human phase I trial.
A novel bromodomain and extra terminal protein (BET) inhibitor demonstrated promising early activity and a manageable safety profile in the treatment of patients with relapsed or refractory lymphoma in the results of a first-in-human phase I trial.
“CPI-0610 is a well-tolerated, oral BET inhibitor. The major [adverse] effect is thrombocytopeniathat is a class effect and it is reversible and noncumulative,” said Adrian Senderowicz, MD, of Constellation Pharmaceuticals, who presented the findings during the 2018 International Congress on Targeted Anticancer Therapies.
CPI-0610 is an oral potent and selective BET bromodomain inhibitor. Senderowicz noted that “the regulation of BET proteins can modulate critical signaling pathways for oncology: MYC, BCL2, NF-kβ target genes, and TGF-β target genes.”
The phase I 0610-01 trial was 1 of 3 phase I studies examining the potential of the BET inhibitor. The dose-escalation study in patients with progressive lymphoma had a 3+3 design and evaluated doses from 6 mg to 300 mg in capsule form and at 125 mg or 225 mg in tablet form. Across all doses, the schedule was 14 days on and 7 days off.
Patients in the study had relapsed or refractory non-Hodgkin or Hodgkin lymphoma who were not eligible for or who had relapsed after high-dose chemotherapy or transplant. The primary endpoint of the study was the maximum-tolerated dose for CPI-0610, and secondary endpoints included safety, tolerability, pharmacokinetics, preliminary antitumor effects, and pharmacodynamics.
Sixty-four patients were included in the trial across the 11 investigated doses. Of these, 75% were male and the median age was 63 years. Most patients were heavily pretreated with a median of 4 prior therapies (range, 1-12).
The majority of the patients (56.3%) had diffuse large B-cell lymphoma, 12.5% had follicular lymphoma, 7.8% had Hodgkin lymphoma, 4.7% had mantle cell lymphoma, and 18.8% had a different lymphoma diagnosis.
The most common (≥5%) treatment-related adverse events across all doses and across both forms of treatment was thrombocytopenia (42.2%), nausea (17.2%), and fatigue (17.2%). No cases of thrombocytopenia were observed in patients who received doses of 50 mg or lower.
The study included a broad view of dose-limiting toxicities (DLTs) (TABLE). Hematologic DLTs were observed in 4 patients, including 1 patient who developed grade 3 neutropenic fever at the 80-mg capsule dose. Grade 4 thrombocytopenia was experienced by 3 patients, including 1 on the 230-mg capsule dose, another on the 300-mg capsule, and a third who was receiving the 225-mg tablet. Two of the 3 patients recovered within 2 weeks.
Nonhematologic DLTs included 1 grade 3 rash at 48 mg, and 2 cases of grade 3 diarrhea, 1 at 170 mg and another at 230 mg. Each of the nonhematologic DLTs were resolved.
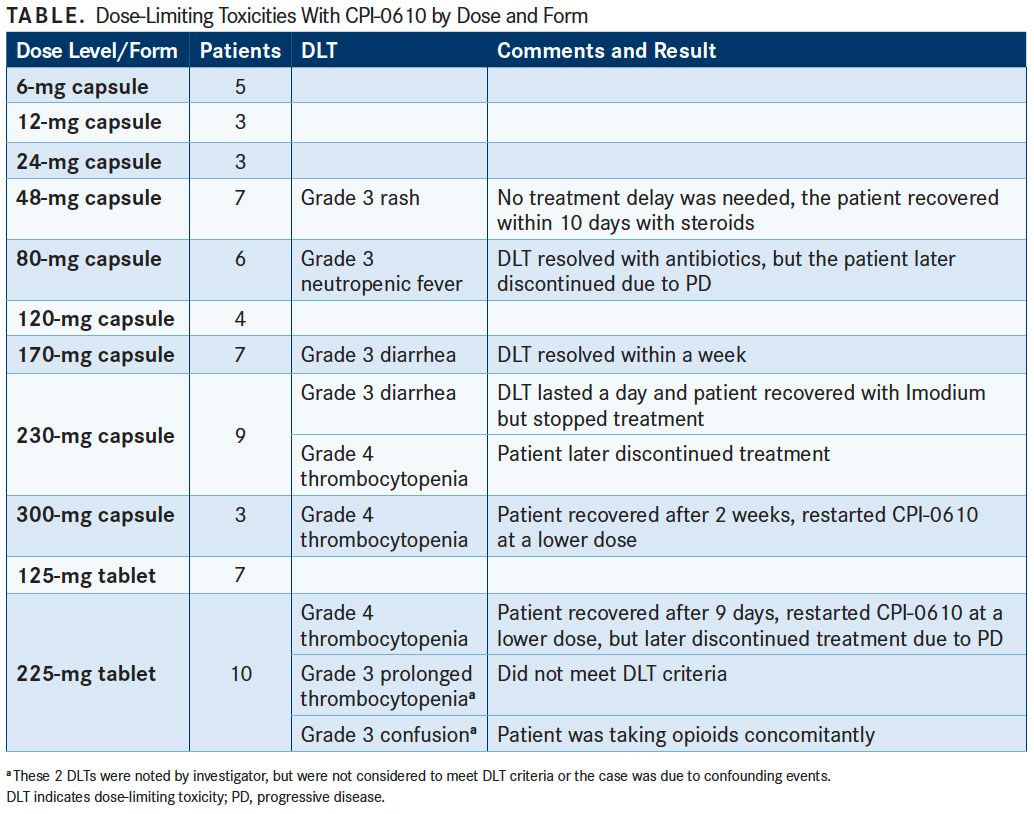
The maximum-tolerated dose was deemed to be 225 mg in tablet form, which was also based on DLTs found in the other phase I studies.
Among 38 patients evaluable for efficacy analysis, 5 objective responses (13.2%) were observed, including 2 complete responses (CRs) and 3 partial responses (PRs). Three of 5 patients with activated B-cell diffuse large B-cell lymphoma experienced a response, consisting of 1 CR and 2 PRs. The second CR was achieved in a patient with T-cell histiocyte rich B-cell lymphoma and 1 patient with follicular lymphoma had a PR. Senderowicz added that 17 other patients experienced some degree of tumor shrinkage.
In the pharmacokinetics analysis of CPI-0610 across the doses studied, the investigators noted dose proportional increases in exposure across the 6-mg to 170-mg capsule doses with similar exposure observed across the 170-mg to 300-mg doses. However, the tablet form was recommended for further investigation. “The bioavailability of the tablets is approximately 40% higher than the capsules,” he said.
IL8 and CCR1 mRNA levels were both evaluated in peripheral blood mononuclear cells for treatment effects. CPI-0610 rapidly suppressed expression of both proinflammatory cytokines. “There is a dose-dependent and concentration-dependent inhibition of IL8 and CCR1, and both are NF-kB dependent genes,” Senderowicz said. Maximal effects were observed 2 hours after treatment.
Based on preclinical data and significant clinical effects on proinflammatory cytokines, a phase II trial has also begun looking at CPI-0610 either with or without ruxolitinib (Jakafi) in myelofibrosis in the second-line setting (NCT02158858).
Reference:
Blum KA, Abramson J, Maris M, et al. A phase I study of CPI-0610, a bromodomain and extra terminal protein (BET) inhibitor in patients with relapsed or refractory lymphoma. Presented at: TAT 2018 Targeted Anticancer Therapies; March 5-7, 2018; Paris, France. Abstract 410.

Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen
Savona Discusses First-Line JAK Inhibition for Patients With Myelofibrosis at Risk of Anemia
April 17th 2024During a Case-Based Roundtable® event, Michael Savona, MD, and participants discussed the case of a patient with myelofibrosis and moderate anemia receiving JAK inhibitor therapy.
Read More