Melanoma Investigators Strive to Overcome PD-1 Inhibitor Resistance
Investigators across the globe have expended considerable effort attempting to identify mechanisms of response and resistance to ICIs. The general conclusion is that each patient’s response to immunotherapy is likely complex and highly individualized.
Jennifer A. Wargo, MD, MMSc
Approximately one-third to one-half of patients with advanced melanoma respond to PD-1 inhibitor therapy, which is superior to response rates observed with systemic chemotherapy or even single-agent ipilimumab (Yervoy)a cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) blocker and the first checkpoint inhibitor approved for melanoma.1-4Nevertheless, a significant proportion of patients have primary, or innate, resistance to PD-1 inhibition and derive no benefit from these therapies that have become the standard of care for advanced melanoma.5In addition, several years have passed since the first patients received PD-1 inhibitors in clinical trials, and it has become clear that although most responses are durable and last several years, one-fourth to one-third of patients relapse despite ongoing treatment.3,6,7These patients are categorized as having secondary, or acquired, resistance.5
The lack of adequate therapies for advanced melanoma that is resistant to immune checkpoint inhibitors (ICIs) remains an important unmet need in this tumor type. To address this problem, investigators across the globe have expended considerable effort attempting to identify mechanisms of response and resistance to ICIs. The general conclusion is that each patient’s response to immunotherapy is likely complex and highly individualized.5
Numerous pathways and patient characteristics have been implicated in poor response to PD-1 inhibition, with more discovered every year.5,8They are broadly divided between tumor-extrinsic, or host, and tumor-intrinsic factors.5Potential host factors include the gut microbiome, diet, the patient’s health and immune status, and other medications or treatments.8Tumor-intrinsic mechanisms include histology, genetic and epigenetic changes in the tumor or its microenvironment (TME), and tumor mutational burden.5,8The wealth of information about resistance mechanisms has inspired the development of many different treatment strategies for preventing or overcoming PD-1 inhibitor resistance, which are being evaluated in ongoing clinical trials.
Gut Microbiome in Immunotherapy Response
Jennifer A. Wargo, MD, MMSc, associate professor in the department of Surgical Oncology and Genomic Medicine at The University of Texas MD Anderson Cancer Center in Houston, runs a research laboratory, and is coleader of MD Anderson’s Melanoma Moon Shot Program. She said the goal of the almost 7-year-old program is to “help end pain and suffering for patients with cancer over the next decade,” and it has supported her extensive research into mechanisms of resistance to ICIs and new treatment approaches. “We’ve made some major discoveries and have been able to run some novel clinical trials that have profoundly improved outcomes for patients with cancer,” she said in an interview with Targeted Therapies in Oncology.
Wargo is particularly excited about her group’s efforts to untangle the relationship between the gut microbiome and responses to ICIs. She explained that the human body contains more than 100 trillion microbes, which is almost 10 times the number of human cells.
“A large proportion of those microbes reside in the gut, which has a huge surface area. On one side, you have all these microbes, and on the other side, you have a dense network of immune cells,” she said. Microbial metabolites facilitate cross talk between microbes and immune cells in the gastrointestinal tract; they also influence immune system functions locally and then systemically as immune cells migrate from the intestines throughout the body via the lymphatic and circulatory systems.9
Wargo said the sheer quantities of microbes and immune cells in the gut and their constant interactions convinced her there is a “tight link between the gut microbiome and response to cancer immunotherapy.” Bolstered by findings from murine and other preclinical studies,9Wargo and colleagues decided to test the theory in humans with metastatic melanoma. They prospectively collected and analyzed samples of the gut microbiome from 112 patients about to start PD-1 inhibitor therapy.10Later, they assessed whether bacterial diversity at baseline corresponded with treatment outcomes. According to Wargo, “Patients who had low diversity of bacteria within the microbiome and a higher abundance of Bacteroidales were far less likely to respond than patients who had what we would characterize as a favorable microbiome, with high diversity and a higher abundance of specific taxa such as Ruminococcaceae or Clostridiales.” Also, immune profiling of the TME revealed that enrichment of these favorable taxa in the microbiome of responders was associated with an increase in the CD8-positive T-cell infiltrate in the tumor.10
Next, they transplanted stool from the treated patients into germ-free mice, which were subsequently injected with melanoma cells and dosed with an antiPD-1 ligand 1 (PD-L1) inhibitor. Mice transplanted with fecal microbiota from the PD-1 responders had significantly greater tumor shrinkage, better responses to the anti–PD-L1 regimen, and a more favorable microbiome than mice that received stool from the nonresponders.10
“We have now gone on to ask, ‘Can we modulate the microbiome and make patients respond better?’” Wargo said. Investigators from MD Anderson and The Angeles Clinic, in collaboration with Seres Therapeutics and the Parker Institute for Cancer Immunotherapy, are currently recruiting patients with advanced melanoma for an ongoing phase Ib clinical trial of therapies designed to alter the microbiome before PD-1 inhibitor therapy (NCT03817125). One group of patients will receive SER-401, an oral capsule that contains fecal bacterial spores consistent with the microbiome signature of responders to anti PD-1 therapy. Both groups will be treated with nivolumab (Opdivo), a PD-1 inhibitor approved for advanced melanoma.
Wargo said she was encouraged by preliminary data presented at the 2019 American Association for Cancer Research (AACR) Annual Meeting from 2 clinical trials of fecal transplant in patients with melanoma.11She described one study that “used a fecal transplant from a complete responder donor, gave that back to patients who had progressed on antiPD-1, and reintroduced checkpoint blockade.” Wargo said the patients responded to retreatment and that “the fecal transplant was associated with an increased infiltrate of favorable immune cells within the tumor microenvironment.”
Another study led by Wargo examined whether certain lifestyle factors influence the microbiome in patients with melanoma. Data were presented at the 2019 AACR Annual Meeting that showed “patients who had a high-fiber diet were about 5 times more likely to respond to treatment with antiPD-1 therapy.”12
Wargo’s group also examined the relationship among baseline use of over-the-counter probiotics, the microbiome signature, and treatment response.12“About 42% of our patients reported taking a probiotic, and strikingly, patients who took a probiotic had lower diversity of their microbiome and were less likely to respond,” Wargo said. The findings suggest that clinicians may want to discuss probiotic use with patients starting immunotherapy.
Overcoming Tumor-Intrinsic Resistance to PD-1 Inhibition
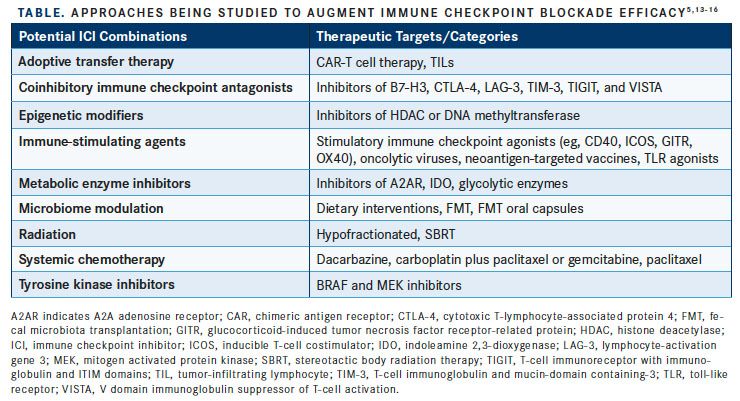
In cancer, chronic antigen exposure leads to exhaustion of CD8-positive tumor-infiltrating lymphocytes (TILs) and upregulation of multiple coinhibitory factors, including PD-1 and PD-L1.13 The success of checkpoint blockade with PD-1/ PD-L1 inhibitors largely depends on their ability to mobilize, reactivate, and expand antigen-specific cytotoxic CD8-positive T lymphocytes.5 Achieving long-term disease control depends on generating a persistent population of effector memory T cells. Defects that lead to loss of T-cell function, limit the expression or recognition of tumor neoantigens, promote an immunosuppressive TME, or facilitate immune escape contribute to treatment failure.5,7 Various strategies to overcome PD-1 resistance or optimize antitumor responses are being evaluated in clinical trials for melanoma and other solid tumors. Several strategies take a combinatorial approach, using a PD-1/ PD-L1 inhibitor as a backbone and adding a novel or existing therapeutic approach (TABLE).13-16
Targeting Coinhibitory Receptors
The FDA has already approved dual checkpoint blockade combining a PD-1 inhibitor (nivolumab) with a CTLA-4 inhibitor (ipilimumab) as a first-line strategy for unresectable or metastatic melanoma based on the pivotal CheckMate 067 trial.17Data from the trial showed that the combination produced a significantly better objective response rate (ORR), median progression-free survival (PFS), and median overall survival (OS) than ipilimumab monotherapy.13
After preclinical data suggested that ICI therapy might be more effective in the neoadjuvant setting versus the adjuvant setting, Wargo and colleagues initiated a phase II trial to evaluate neoadjuvant use of the ipilimumab/nivolumab combination in patients with high-risk melanoma. The combined approach produced a higher RECIST overall response rate than nivolumab monotherapy (73% vs 25%, respectively) and a higher rate of pathologic complete response (45% vs 25%, respectively). However, the study ended prematurely because of the 73% rate of grade 3 toxicity in the combination arm.18
Wargo said despite the disappointing outcome, they succeeded in identifying a possible biomarker of response. “Everyone is looking for the holy grail of biomarkers, and a lot of the focus has been on cytotoxic T cells,” she said, adding, “What we found were major differences in B cells between responders and nonresponders to immune checkpoint blockade.”
Responders had higher proportions of class-switched memory B cells and plasma-like cells, whereas nonresponders had a higher proportion of naïve B cells.19Switched B cells have been activated to produce a specific class of antibodies, whereas naïve B cells have not yet been activated. Wargo said, “We found that these B cells were actually forming little lymph nodes within the patient’s tumor.” She said that although they determined that activated effector B-cell phenotypes contributed to response, other studies have reported that B cells were detrimental to response. Wargo said she hoped more research into biomarkers of ICI response would look beyond T cells to include B cells and other immune cell subtypes.
Wargo said an important goal of investigators is to improve the safety of regimens that combine ICIs. She noted that the OpACIN-neo trial also evaluated neoadjuvant ipilimumab/nivolumab in melanoma and found that “you can reduce the dose of the CTLA-4 inhibitor and increase the dose of the PD-1 inhibitor to lower the toxicity while preserving the response.”20 She praised the multinational study as an example of what global cooperation can achieve and stressed the importance of “breaking down silos” between investigators in melanoma. Recently, Wargo and other melanoma experts around the world formed the International Neoadjuvant Melanoma Consortium to advance neoadjuvant melanoma research. They plan to meet in June at the 2019 American Society of Clinical Oncology Annual Meeting.
Lymphocyte-activation gene 3 (LAG-3) is another coinhibitor expressed on various immune cells in the TME, including on the surface of CD8-positive and CD4-positive T cells. LAG-3 is often coexpressed with PD-1 and exacerbates T-cell exhaustion.13Preclinical and early-phase trial data suggest that inhibitors of LAG-3 and PD-1 work synergistically to reactivate T cells.13A phase I/II study evaluated combinatorial therapy with the LAG-3 inhibitor relatlimab (BMS-986016) and nivolumab in heavily pretreated patients with advanced melanoma. The ORR was 11.5%, with patients with ≥1% of tumor cells positive for LAG-3 expression significantly more likely to respond.21The regimen was well tolerated and is now being studied in a phase II/III trial as first-line therapy for advanced melanoma (NCT03470922). Several ongoing clinical trials are evaluating regimens that combine PD-1 inhibitors with novel ICIs that target other coinhibitory receptors.
Immune-Stimulating Agents Plus PD-1 Inhibition
Instead of blocking pathways that inhibit immune function, immune-stimulating agents amplify immune responses and may act synergistically with PD-1/PD-L1 inhibitors.13Multiple clinical trials are investigating regimens that combine an ICI with a stimulatory checkpoint agonist. Stimulatory checkpoints are molecules that enhance innate and adaptive antitumor immune responses by improving immunologic memory; promoting T-cell activation, differentiation, and proliferation; and boosting T-cell effector function.13,22Oncolytic viruses, toll-like receptor (TLR) agonists, and anticancer vaccines are other types of immune-stimulating agents being paired with ICIs in clinical trials.5
The monoclonal antibody APX005M is a CD40 agonist being investigated with nivolumab for advanced melanoma that has progressed during antiPD-1 therapy, and data from a phase I/II clinical trial of the doublet were presented at the 2019 AACR Annual Meeting. Only 1 of 5 patients with melanoma in the phase I trial responded, achieving a partial response (PR). In the phase II trial, which included 10 patients, investigators documented 2 PRs and no complete responses (CRs). The regimen was well tolerated, and recruitment for the phase II trial is ongoing.23
In a phase Ib/II trial, the TLR9 agonist SD-101 was administered with pembrolizumab (Keytruda) to patients with advanced melanoma who were naïve to PD-1 inhibitors. The ORR for the 25 participants who completed at least 15 weeks of therapy was 60% (CR, 12%), and the disease control rate (DCR) was 76%. The combination was well tolerated and did not increase the risk of immune-related adverse events (irAEs).24
The oncolytic virus T-VEC (talimogene laherparepvec [Imlygic]), a modified herpes simplex virus type 1 approved for advanced melanoma, expresses granulocyte-macrophage colony-stimulating factor to increase tumor-specific antigen presentation by dendritic cells at the injection site, thus creating antigen-specific CD8-positive T cells for the PD-1 inhibitor to reactivate and proliferate. In the phase Ib portion of the MASTERKEY-265 trial, 21 patients with advanced melanoma received single-agent T-VEC followed by a combination of T-VEC and pembrolizumab.22The ORR was 62%, and the CR rate was 33%. Even some patients with a low density of CD8- positive TILs or no IFN-γ gene signature at baseline achieved responses, suggesting that T-VEC turned cold, or nonT-cell inflamed, tumors into hot tumors.
Biopsies after the T-VEC run-in phase showed increases over baseline in the density of infiltrating CD8-positive T cells and upregulated PD-1 expression. Upregulation of PD-1, combined with PD-L1 expression by tumor cells, likely inhibited the antitumor activity of single-agent T-VEC at distant sites. Concurrent PD-1 blockade overcame PD-L1induced resistance to oncolysis in the TME, however, and freed effector T cells to migrate to distant sites.22The findings provide a logical rationale for combining the 2 treatment modalities, and the combination is being studied further in the phase III KEYNOTE-034 trial (NCT02263508).
PD-1 Inhibition With Epigenetic Modulation
Drugs that inhibit DNA methylation or histone deacetylation (HDAC) sensitize cancer cells to ICIs in part by increasing expression of tumor-specific antigens and costimulatory molecules as well as upregulating TIL expression of PD-1/PD-L1.25The novel HDAC inhibitor entinostat (SNDX-275) also impairs the function of myeloid-derived suppressor cells, which cause immunosuppression in the TME.5,13At the 2019 AACR Annual Meeting, investigators presented preliminary findings from ENCORE-601, a clinical trial that paired entinostat with pembrolizumab.26The study included 53 patients with advanced melanoma who progressed during or after treatment with a PD-1 inhibitor; 70% had also used ipilimumab. The ORR with entinostat plus pembrolizumab was 19%, the median duration of response at data cutoff was 12.5 months, and the median PFS was 4.2 months. The most common grade 3/4 AEs were neutropenia, fatigue, and hyponatremia; only 5 patients experienced grade 3/4 irAEs.26
Adoptive Cell Therapy With TILs
Multiple clinical trials are evaluating the efficacy and safety of combining adoptive cell therapy (ACT) using TILs with a PD-1 inhibitor for patients with advanced melanoma.15One of the main focuses for TILs is in patients with melanoma who did not benefit from antiPD-1 therapy. Data were presented in November 2018 from a phase II trial of lifileucel (LN-144), an investigational cryopreserved autologous TIL therapy, in patients with metastatic melanoma that progressed despite PD-1 inhibitor therapy.27The multinational trial enrolled 47 patients, who were infused with manufactured TILs derived from a sample of their tumor. Before infusion, patients underwent nonmyeloablative lymphodepletion; after infusion, they received up to 6 doses of interleukin-2.27,28
The ORR was 38% and included 1 CR; 38% of patients also achieved stable disease, which resulted in a DCR of 77%.26The median duration of response was 6.4 months (range, 1.3-14 months). Almost all the responders (16/17) had not responded to prior treatment with a PD-1 inhibitor. Hematologic toxicities grade ≥3 were common, with high rates of thrombocytopenia (81%), neutropenia (53%), febrile neutropenia (53%), and anemia (47%). The study is ongoing and has already started recruiting patients for an expanded cohort that will include 80 to 100 participants.27
References:
- Weber JS, D'Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384. doi: 10.1016/S1470-2045(15)70076-8.
- Weber JS, Gibney G, Sullivan RJ, et al. Sequential administration of nivolumab and ipilimumab with a planned switch in patients with advanced melanoma (CheckMate 064): an open-label, randomised, phase 2 trial. Lancet Oncol. 2016;17(7):943-955. doi: 10.1016/S1470-2045(16)30126-7.
- Schachter J, Ribas A, Long GV, et al. Pembrolizumab versus ipilimumab for advanced melanoma: final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006). Lancet. 2017;390(10105):1853-1862. doi: 10.1016/S0140-6736(17)31601-X.
- Ribas A, Hamid O, Daud A, et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA. 2016;315(15):1600-1609. doi: 10.1001/jama.2016.4059.
- Jenkins RW, Barbie DA, Flaherty KT. Mechanisms of resistance to immune checkpoint inhibitors. Br J Cancer. 2018;118(1):9-16. doi: 10.1038/bjc.2017.434.
- Hamid O, Hersey P, Wolchok JD, et al. Five-year survival outcomes for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001 [published online January 31, 2019]. Ann Oncol. doi: 10.1093/annonc/mdz011.
- Sharma P, Hu-Lieskovan S, Wargo JA, Ribas A. Primary, adaptive, and acquired resistance to cancer immunotherapy. Cell. 2017;168(4):707-723. doi: 10.1016/j.cell.2017.01.017.
- Seto T, Sam D, Pan M. Mechanisms of primary and secondary resistance to immune checkpoint inhibitors in cancer. Med Sci (Basel). 2019;7(2):14. doi: 10.3390/medsci7020014.
- Gopalakrishnan V, Helmink BA, Spencer CN, Reuben A, Wargo JA. The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell. 2018;33(4):570-580. doi: 10.1016/j.ccell.2018.03.015.
- Gopalakrishnan V, Spencer CN, Nezi L, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 2018;359(6371):97-103. doi: 10.1126/science.aan4236.
- Baruch E, Youngster I, Ortenberg R, et al. Fecal microbiota transplantation (FMT) and re-induction of anti-PD-1 therapy in refractory metastatic melanoma patients - preliminary results from a phase I clinical trial (NCT03353402). 2019 American Association for Cancer Research Annual Meeting; March 29-April 3, 2019; Atlanta, Georgia. bit.ly/2UllVqr.
- Spencer C, Gopalakrishnan V, McQuade J. The gut microbiome (GM) and immunotherapy response are influenced by host lifestyle factors. 2019 American Association for Cancer Research Annual Meeting; March 29-April 3, 2019; Atlanta, Georgia. Abstract 2838/24. https://bit.ly/2VCJQxB.
- Popovic A, Jaffee EM, Zaidi N. Emerging strategies for combination checkpoint modulators in cancer immunotherapy. J Clin Invest. 2018;128(8):3209-3218. doi: 10.1172/JCI120775.
- Khair DO, Bax HJ, Mele S, et al. Combining immune checkpoint inhibitors: established and emerging targets and strategies to improve outcomes in melanoma. Front Immunol. 2019;10:453-453. doi: 10.3389/fimmu.2019.00453.
- Rohaan MW, van den Berg JH, Kvistborg P, Haanen JBAG. Adoptive transfer of tumor-infiltrating lymphocytes in melanoma: a viable treatment option. J Immunother Cancer. 2018;6(1):102. doi: 10.1186/s40425-018-0391-1.
- Eggermont AMM, Crittenden M, Wargo J. Combination immunotherapy development in melanoma. Am Soc Clin Oncol Ed Book. 2018:197-207. doi: 10.1200/edbk_201131.
- Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2017;377(14):1345-1356. doi: 10.1056/NEJMoa1709684.
- Amaria RN, Reddy SM, Tawbi HA, et al. Neoadjuvant immune checkpoint blockade in high-risk resectable melanoma. Nat Med. 2018;24(11):1649-1654. doi: 10.1038/s41591-018-0197-1.
- Reddy S, Helmink B, Gao J. Effector B cells and tertiary lymphoid structures predict response to immune checkpoint blockade in solid tumors. 2019 American Association for Cancer Research Annual Meeting; March 29-April 3, 2019; Atlanta, Georgia. Abstract 4488. https://bit.ly/2Vg845q.
- Blank CU, Rozeman EA, Klop WMC, et al. OpACIN-neo: a multicenter phase II study to identify the optimal neo-adjuvant combination scheme of ipilimumab (IPI) and nivolumab (NIVO). Ann Oncol. 2018;29(suppl 8; abstr LBA42). doi: 10.1093/annonc/mdy424.052.
- Ascierto PA, Bono P, Bhatia S, Melero I, Nyakas M, Svane I. Efficacy of BMS-986016, a monoclonal antibody that targets lymphocyte activation gene-3 (LAG-3), in combination with nivolumab in pts with melanoma. Ann Oncol. 2017;28(suppl 5):v605-v649. doi: 10.1093/annonc/mdx440.
- Ribas A, Dummer R, Puzanov I, et al. Oncolytic virotherapy promotes intratumoral T cell infiltration and improves anti-PD-1 immunotherapy. Cell. 2017;170(6):1109-1119.e1110. doi: 10.1016/j.cell.2017.08.027.
- Kluger H, Weiss S, Olszanski A. Phase Ib/II of CD40 agonistic antibody APX005M in combination with nivolumab (nivo) in subjects with metastatic melanoma (M) or non-small cell lung cancer (NSCLC). 2019 American Association for Cancer Research Annual Meeting; March 29-April 3, 2019; Atlanta, Georgia. Abstract CT089. https://bit.ly/2ZTrdsy
- Ribas A, Milhem MM, Hoimes CJ, et al. Phase 1b/2, open label, multicenter, study of the combination of SD-101 and pembrolizumab in patients with advanced melanoma who are naïve to anti-PD-1 therapy. J Clin Oncol. 2018;36(suppl 15; abstr 9513). doi: 10.1200/JCO.2018.36.15_suppl.9513.
- Dunn J, Rao S. Epigenetics and immunotherapy: the current state of play. Mol Immunol. 2017;87:227-239. doi: 10.1016/j.molimm.2017.04.012.
- Sullivan R, Moschos S, Johnson M. Efficacy and safety of entinostat (ENT) and pembrolizumab (PEMBRO) in patients with melanoma previously treated with anti-PD1 therapy. 2019 American Association for Cancer Research Annual Meeting; March 29-April 3, 2019; Atlanta, Georgia. Abstract CT072. https://bit.ly/2I0iPSd.
- Sarnaik A, Thomas S, Davar D. Safety and efficacy of cryopreserved autologous tumor infiltrating lymphocyte therapy (LN-144, lifileucel) in advanced metastatic melanoma patients following progression on checkpoint inhibitor. 2018 Society for Immunotherapy of Cancer Annual Meeting; November 7-11, 2018; Washington, DC. https://bit.ly/2ZNZV6B.
- Sarnaik A, Curti BD, Davar D, et al. A phase 2, multicenter study to assess the efficacy and safety of autologous tumor-infiltrating lymphocytes (LN-144) for the treatment of patients with metastatic melanoma. J Clin Oncol. 2018;36(suppl 15; abstr TPS9595). doi: 10.1200/JCO.2018.36.15_suppl.TPS9595.

Management of Immune-Related Toxicities in Melanoma Has Improved Over Time
April 24th 2024During a Case-Based Roundtable® event, Evan J. Lipson, MD, discussed with participants how their experience with immunotherapy toxicities has changed over time in the first article of a 2-part series.
Read More
Novel Approaches Focus on Limiting Toxicity in Older Patients With ALL
April 22nd 2024The major challenges for clinicians treating older patients with acute lymphoblastic leukemia surround the emergence of resistance to existing therapies and the toxicities associated with current chemotherapies.
Read More