Biomarkers for Checkpoint Inhibitor Induced Diabetes Are Necessary for irAE Management
Certain patients with cancer who are treated using immune checkpoint inhibitors may develop a form of insulin-dependent diabetes that is associated with immune-related adverse events resulting from therapy, according to research published in <em>The Lancet Diabetes & Endocrinology</em>.
Ana Luisa Perdigoto, MD, PhD

Ana Luisa Perdigoto, MD, PhD
Certain patients with cancer who are treated using immune checkpoint inhibitors may develop a form of insulin-dependent diabetes that is associated with immune-related adverse events (irAEs) resulting from therapy, according to research published inThe Lancet Diabetes & Endocrinology.1
“Provider and patient awareness of this new form of insulin-dependent diabetes is important for early identification and appropriate clinical care,” Ana Luisa Perdigoto, MD, PhD, and colleagues wrote in their report. “Studies to identify features of patients that might serve as biomarkers of risk and mechanisms are objectives of ongoing studies.”
Several mechanisms may play a role in checkpoint inhibitorinduced diabetes, which occurs most frequently following treatment with PD-1/ PD-L1 or CTLA-4 inhibitors. Endocrinopathies resulting from immunotherapy may include insulin-producing b cells of the pancreas as well as dysfunction in the pituitary, thyroid, and adrenal glands. Prior studies have also demonstrated the potential of PD-L1 to protect against the development of autoimmune diabetes.2
Often, patients who develop type 1 diabetes mellitus will first present with diabetic ketoacidosis or severe hyperglycemia.3 Roughly 0.9% of patients treated with checkpoint inhibitors will subsequently develop diabetes, most frequently those with malignant melanoma.1
Recent Study Data
In 2 studies that included 64 patients with checkpoint inhibitorinduced diabetes across at least 13 different tumor types, onset was typically acute with a sudden increase in blood glucose levels.
The median time from initiation of immunotherapy to the diagnosis of diabetes was reported as 11 weeks (range, 1-228) and the mean glycated hemoglobin (A1c) was 7.9% at diagnosis. However, the A1c range5.8% to 10.7%—could reflect either high levels of glucose at the time of onset or a period of latent glucose intolerance.
Seventy-five percent of patients had diabetic ketoacidosis and 91% had low or undetectable C-peptide levels. Patients with diabetic ketoacidosis and autoantibodies diagnostic of spontaneous type 1 diabetesincluding glutamic acid decarboxylase 65, islet antigen 2, zinc transporter 8, and insulin autoantibodies—had shorter disease onset than those who did not have these prognostic features. Inflammation in the exocrine pancreas might have played a role in the disease process in certain patients, based on the rate of elevated lipase/amylase that occurred in 32%. There was also a robust correlation between HLA-DR4 haplotypes and disease onset, occurring in 62% of patients.
Methods of irAE Control
Continuous glucose monitoring may help to avoid hyperglycemia since glucose levels can fluctuate greatly in checkpoint inhibitorinduced diabetes. Perdigoto et al suggested that A1c targets could be relaxed in older patients, with monitoring for the purposes of avoiding hypoglycemia, ketoacidosis, symptomatic hyperglycemia, and risk of infection (FIGURE).1,4
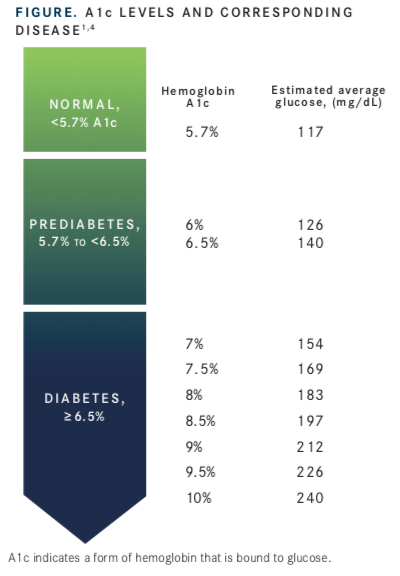
“Among the 17 patients currently being followed in our clinics, the mean A1c is 7.8% (standard deviation, SD = 1.3%) after a mean of 110 weeks (SD = 59; range, 23-258) on insulin therapy,” Perdigoto et al noted.
Additionally, immune checkpoint inhibitors in patients with type 2 diabetes whose disease worsens might also be affected by this irAE, leading the investigators to conclude that further studies are needed in this population.
Anecdotal evidence suggests that the effects of this irAE may be irreversible, possibly because of rapid loss of b cells or the damaging effect of steroids on b-cell function. Patients with checkpoint inhibitorinduced diabetes will require insulin therapy in almost all cases, and severe instances of hypoglycemia have occurred in this patient population. Therefore, it is essential that patients be informed of the risks of developing this permanent irAE.
The investigators said a better understanding of biomarkers that lead to checkpoint inhibitorinduced diabetes may make it possible to prevent this irAE without adversely affecting the agents’ antitumor effects. In addition, past research has suggested that the presence of irAEs may serve as a predictive biomarker of response to immunotherapy, but the association remains uncertain. Studies for identifying patient characteristics that may serve as predictive biomarkers of irAE risk and tumor response are objectives of ongoing studies.
References
- Perdigoto AL, Quandt Z, Anderson M, Herold KC. Checkpoint inhibitor-induced insulin-dependent diabetes: an emerging syndrome.Lancet Diabetes Endocrinol. 2019;7(6):421-423. doi: 10.1016/S2213-8587(19)30072-5.
- Wang CJ, Chou FC, Chu CH, et al. Protective role of programmed death 1 ligand 1 (PD-L1) in nonobese diabetic mice: the paradox in transgenic models.Diabetes. 2008;57(7):1861-1869. doi: 10.2337/db07-1260.
- Byun DJ, Wolchok JD, Rosenberg LM, Girotra M. Cancer immunotherapy immune checkpoint blockade and associated endocrinopathies.Nat Rev Endocrinol.2017;13(4):195-207. doi: 10.1038/nrendo.2016.205.
- Understanding A1c. American Diabetes Association website. bit.ly/ 2HcmE4N. Accessed August 16, 2019.

Novel Approaches Focus on Limiting Toxicity in Older Patients with ALL
April 22nd 2024The major challenges for clinicians treating older patients with acute lymphoblastic leukemia surround the emergence of resistance to existing therapies and the toxicities associated with current chemotherapies.
Read More
Ornstein Advises on Starting Dose and Management of Lenvatinib in RCC
April 21st 2024During a Case-Based Roundtable® event, Moshe Ornstein, MD, MA, provided guidance on dosing and toxicity concerns in a patient treated with lenvatinib plus pembrolizumab for advanced renal cell carcinoma.
Read More
Peers Discuss Role of Pola-R-CHP vs R-CHOP in Newly Diagnosed DLBCL
April 19th 2024During a Case-Based Roundtable® event, Haifaa Abdulhaq, MD discussed with participants whether the POLARIX trial influences their choice to use the pola-R-CHP as opposed to R-CHOP regimen for patients with newly diagnosed diffuse large B-cell lymphoma.
Read More