Barriers to Next-Generation Sequencing and Biomarker Testing Remain in NSCLC and CRC
Investigators recommend that genomic testing be adopted to be a reflexive and natural step in evaluating patients with non–small cell lung cancer and colorectal cancer/

Black patients with metastatic non–small cell lung cancer (mNSCLC), metastatic colorectal cancer (mCRC), and metastatic breast cancer (mBC) were less likely to undergo next-generation sequencing (NGS) testing after their diagnosis than their White counterparts, according to an analysis of a real-world database that represents community practices in the United States.1 In particular, the analysis revealed that 29.7% of Black/African Americans undergo NGS testing in nonsquamous NSCLC (NS-NSCLC) compared with 36.6% of White patients. Given the large number of actionable biomarkers and targeted treatments available and that early intervention with targeted treatments leads to positive outcomes, these findings suggest the need for further research in the future.
A total of 14,768 patients were evaluated from the Flatiron Health electronic health record database, and investigators reported that 66.3% of White patients and 8.7% of Black patients comprised the overall population. White patients and Black patients with NS-NSCLC made up 64.9% and 8.9% of the cohort, respectively. In the mCRC cohort, 61.0% were White patients and 10.6% were Black patients, and in the mBC cohort, 62.8% were White patients and 11.2% were Black patients. Black patients in the mNSCLC cohort were more likely to be diagnosed with advanced/metastatic disease, be a younger age, and have been treated in practices in southern states (all P < .0001).
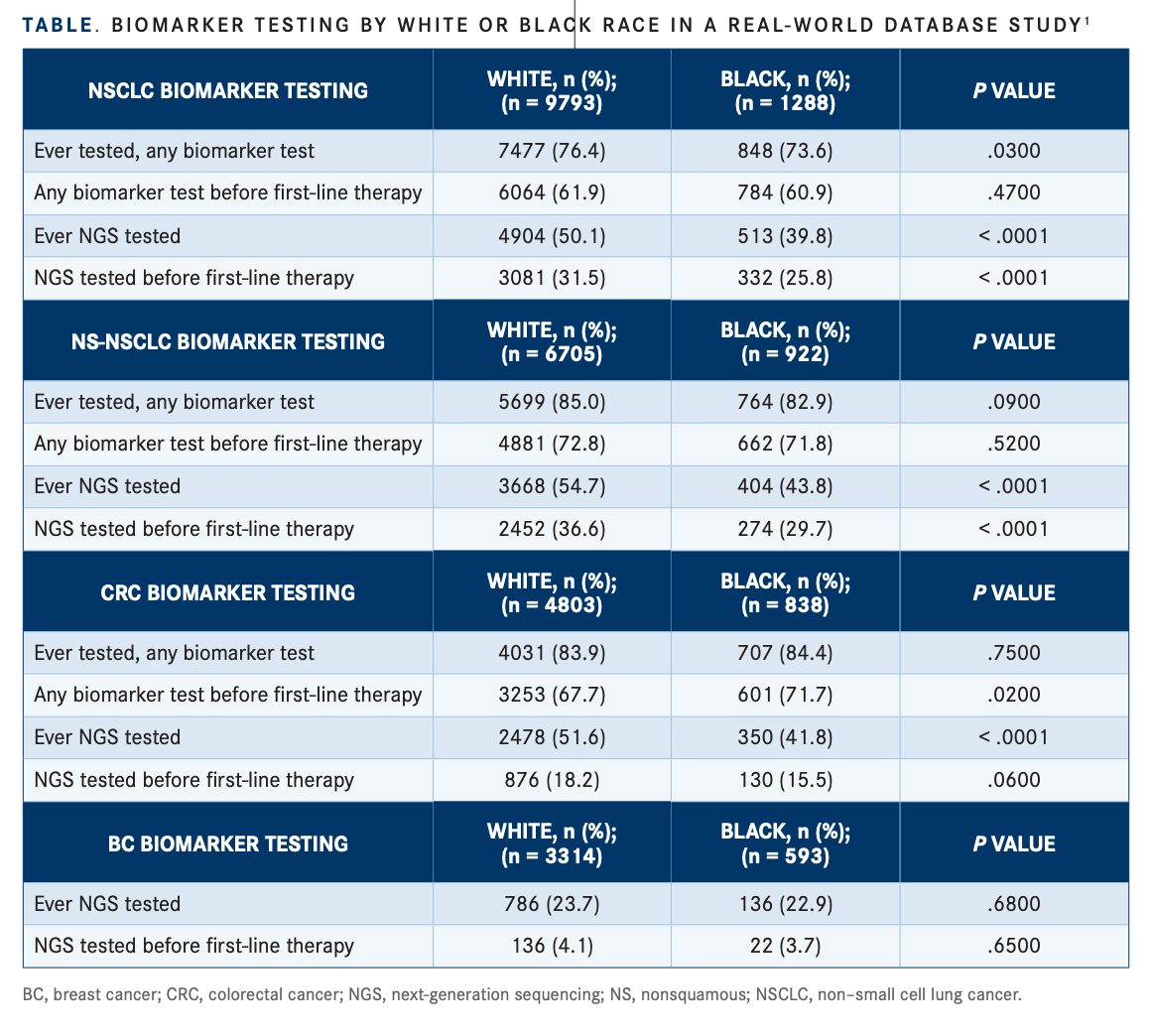
Investigators reported that only 35.5% of patients with NS-NSCLC received NGS testing before first-line therapy was started, and biomarker testing differences before firstline therapy were not statistically signifi cant in either lung cancer cohort for White or Black patients, respectively: 61.9% vs 60.9% in the mNSCLC cohort and 72.8% vs 71.8% in NS-NSCLC cohort (TABLE).1 In the NS-NSCLC cohort, age, performance status, sex, stage at diagnosis, size of the clinical practice where patient received care, smoking status, and race were all signifi cant according to logistic regression (all P < .05).1
In mCRC, investigators observed signifi cant differences in biomarker testing between White and Black patients before the start of fi rst-line therapy: 67.7% vs 71.1%, respectively (P = .02). However, rates of ever receiving biomarker testing were similar between White and Black patients with mCRC: 83.9% vs 84.8%, respectively (P = .75). In the mCRC cohort, factors associated with age, site of disease, performance status, stage at diagnosis, geographic region, and race were all signifi cant (all P < .05).1
Regarding use of targeted therapy, in the mNSCLC cohort, 10.2% of White patients and 9.2% of Black patients received treatment in the front line (P = .24). In the NS-NSCLC cohort, use of targeted therapies was similar for White and Black patients, respectively (14.3% vs 12.3%; P = .09). The use of targeted therapy in the front line was not significant in the mCRC population for White vs Black patients, respectively (4.4% vs 3.6%; P = .28) or in the mBC population (11.4% vs 12.3%; P = .54).1
Clinical Trial Participation The investigators also reviewed the relationship between biomarker testing and clinical trial participation. They noted a statistically signifi cant relationship between biomarker testing and clinical trial enrollment for all cohorts. Black race was a statistically significant covariate in the regression analysis in the overall and NS-NSCLC cohort, but it was not signifi cant for the mCRC or mBC cohort.1
before first-line therapy and at any time were signifi cantly associated with clinical trial participation in the overall mNSCLC and NS-NSCLC cohorts (P ≤ .0001). Findings were similarly signifi cant in the biomarker and NGS-based testing before fi rst-line therapy or at any time in patients with CTC (all P ≤ .0004). In the mBC cohort, only NGS-based testing remained signifi cant (P < .0001).1
Using NGS-based testing is fundamental to determining the most effective approaches for different genomic and immunologic subtypes of tumors. Findings from this study reveal the vast underutilization of comprehensive genomic testing. In the overall mNSCLC cohort, only 76.5% of all patients received biomarker testing, and among those with metastatic NS-NSCC, only 85.0% ever had evidence of a biomarker test.1
Although comprehensive testing could lead to improved patient outcomes, access remains a barrier to many populations. The investigators recommended that genomic testing be adopted to be a refl exive and natural step in evaluating patients.
REFERENCE
1. Bruno DS, Hess LM, Li X, Su EW, Patel M. Disparities in biomarker testing and clinical trial enrollment among patients with lung, breast, or colorectal cancers in the United States. JCO Precis Oncol. 2022;6:e2100427. doi:10.1200/PO.21.00427

Bispecific Antibodies and ADCs Deliver a Futuristic Horizon Across Lung Cancer Settings
October 23rd 2024Recent advancements in protein engineering, especially antibody-drug conjugates, show promise in lung cancer treatment, with ivonescimab outperforming pembrolizumab in PD-L1-positive advanced non-small cell lung cancer.
Read More