Positive Outcomes With Immunochemotherapy and Lenalidomide TP53WT MCL
Findings from a phase 2 study show that sequential minimal residual disease assessment is a powerful prognostic tool in patients with mantle cell lymphoma.
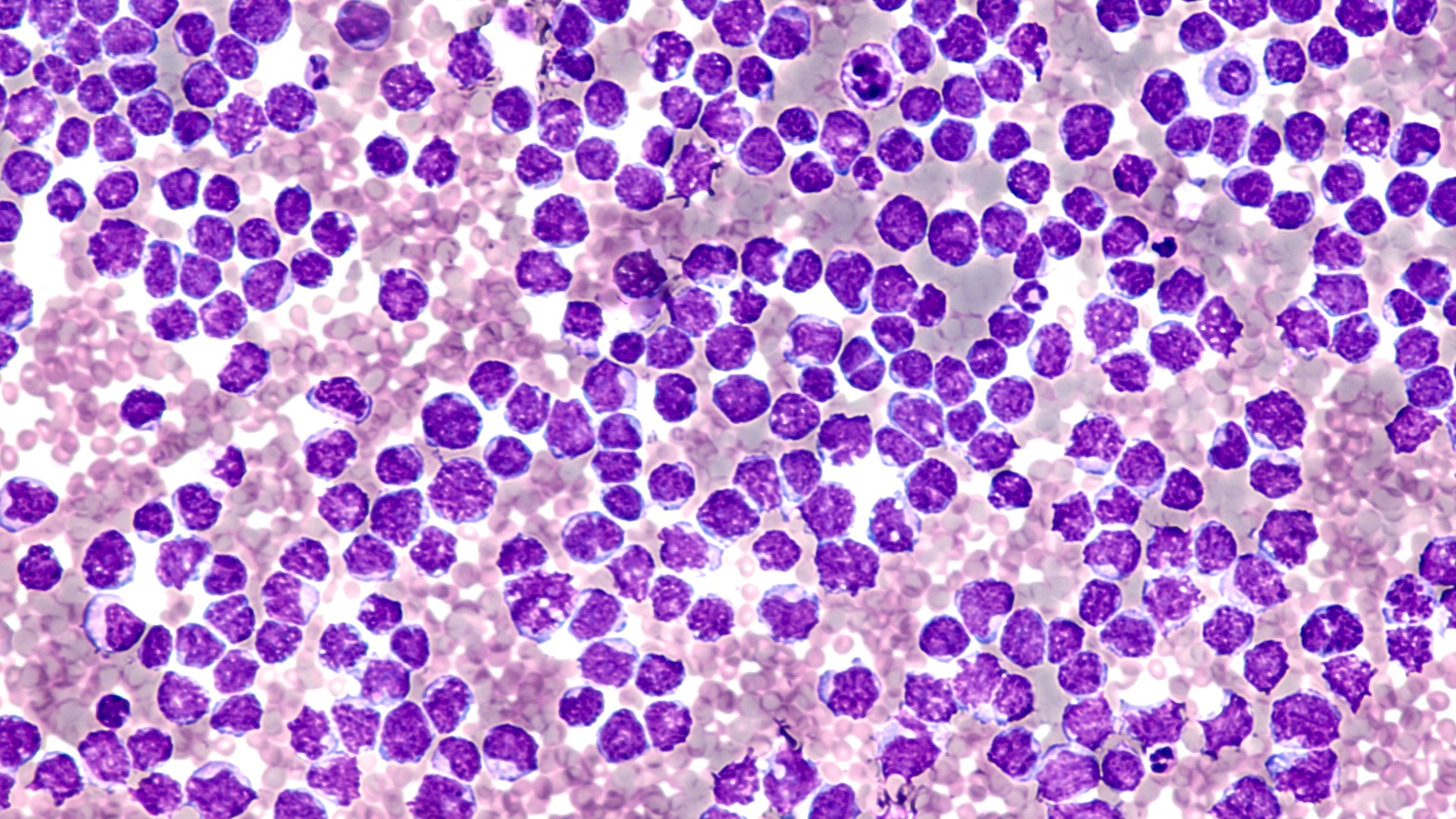
malignant cells of a mantle cell lymphoma: © David A Litman - stock.adobe.com
While the primary end point of 3-year progression-free survival (PFS) was not met, favorable outcomes were observed with immunochemotherapy with lenalidomide (Revlimid), without autologous stem cell transplant consolidation among patients with TP53-wild-type mantle cell lymphoma (MCL), including patients who are at high-risk, according to data from a phase 2 study (NCT02633137) published in Haematologica.1
The median follow-up among survivors was 63 months (range, 11-, 84). By intent-to-treat, the overall response rate was 88% (n = 43) and were all complete responses, including 1 patient who had stable disease, and 2 patients who had disease progression during the study.
The 3-year PFS rate was 63% (95% CI, 50-78), not meeting the study's primary end point, and differed by TP53 status with 78% wild-type vs 38% ALT (P =.043). The median overall survival (OS) at 3 years was 85% (95% CI, 76-96).
“Although the primary study end point of 3-year PFS was not met, this was primarily driven by the poor outcomes observed among patients with TP53-aberrant MCL, further establishing that TP53-aberrant MCL is associated with poor outcomes when treated with [immunochemotherapy] and lenalidomide does not overcome this negative prognostic impact,” wrote study authors in findings published in Haematologica.
In the single-center, investigator-initiated, phase 2 study, patients aged ≥ 18 years with untreated stage II-IV MCL were enrolled if they had radiographically measurable disease, absent active infection, absent central nervous system involvement by MCL, and adequate performance status, blood counts, and organ function.2
A total of 49 patients were enrolled from January 2016 to June 2018, and those who were efficacy-evaluable completed lenalidomide combined with rituximab (Rituxan) plus cyclophosphamide, doxorubicin, vincristine, and prednisone (len-R-CHOP) treatment. Two patients did not complete len-R-CHOP: , 1 for progressive disease, and 1 for toxicity. One patient withdrew from the study in remission following rituximab and cytarabine (R-HiDAC) to pursue high-dose therapy with autologous stem cell rescue.1
Among those enrolled, the median age was 63 years (range, 30-79), 22 (45%) patients were ≥65 years old at enrollment, and 31 (65%) patients were high-risk by protocol. This included 4 patients with blastoid histology. For mutations, 41 (84%) patients had tumor TP53 mutation and deletion status, 14 of which were TP53 aberrant (34%). Three of these patients harbored mutated TP53, 5 harbored one copy of TP53, and 6 patients harbored both. Forty-seven patients ended up being response evaluable.
The primary end point was the rate of PFS at 3 years. Minimal residual disease (MRD) was measured using a next-generation sequencing (NGS)-based assay after each phase of treatment and at 6 months following end-of-treatment.
Additional findings showed that all but 3 response-evaluable patients with localized relapsed MCL amenable to radiation were given BTKi-based therapy. Eight received single-agent and 18 combination therapy, and 19 (76% of response-assessed) patients had disease response.
Nine patients had TP53 mutation at relapse and received BTKi. Of these patients, 7 (78%) experienced disease response. For patients who were relapsing/progressing, the median OS was 32 months (95% CI, 19-not reached [NR]) from time of relapse/progression. Further, the 7 patients who progressed within 2 years of diagnosis had a median OS of 17 months (95% CI, 7-NR) after the 2-year time point vs a median that was not reached for the 38 non-progressing patients (P <.001).
For safety, no treatment-related deaths were observed in the study. The most common grade ≥3 toxicities were hematologic with the most frequent being neutropenia, which occurred in 37% of patients undergoing len-R-CHOP, 70% of patients undergoing R-HiDAC, and 42% of patients receiving R-len. Rates of febrile neutropenia occurred in 14%, 21%, and 7%, and grade ≥3 thrombocytopenia was seen in 22%, 83%, and 9% in the 3 treatment phases, respectively.
Treatment-related adverse events led to dose reductions or delays in 41% of patients receiving len-R-CHOP, 36% treated with R-HiDAC, and 53% given R-len. Twenty patients required dose reduction/delay during len-R-CHOP due to neutropenic fever (n = 7), cytopenia (n = 7), infection (n = 3), rash (n = 2), or other causes (n = 2).
Moreover, rare grade ≥3 infections occurred, including pneumonia (n = 4), skin/soft tissue (n = 1), and sepsis (n = 1), and frequent grade ≤2 toxicities across phases of treatment included fatigue (35% during len-R-CHOP), peripheral sensory neuropathy (29% during len-R-CHOP), and rash (20% during both len-R-CHOP and R-len).
Of the 37 patients with MRD results at the level of 1 x 10-5 sensitivity at end of treatment, 4 were detectable MRD (dMRD), 2 of which were simultaneous with relapse. All 6 patients whose MCL was uMRD at the level of 1 x 10-6 sensitivity at end of treatment converted to dMRD at 6 months post-end of treatment eventually experienced disease relapse. For the 29 patients with level of 1 x 10-6 sensitivity results, including 12 dMRD and 17 undetectable MRD, median PFS was 42 months (95% CI, 34-NR) for uMRD vs 11 months (95% CI, 0-NR) for dMRD (P < .001).
In a high-dose, therapy-sparing, intensive approach, favorable outcomes were seen in patients with TP53-wild-type MCL, including high-risk cases. These data demonstrate that sequential MRD assessment is a powerful prognostic tool in patients with MCL.
“Overall, we have shown that MRD status carried prognostic importance in our sequential treatment regimen, especially at later time points such as 6 months following end of treatment, and that 1 x 10-6 is more strongly predictive of outcomes than 1 x 10-5 sensitivity,” concluded the study authors.
REFERENCES:
Epstein-Peterson ZD, Drill E, Aypar U, et al. Immunochemotherapy plus lenalidomide for high-risk mantle cell lymphoma with measurable residual disease evaluation [published online ahead of print, 2023 Aug 31]. Haematologica. 2023;10.3324/haematol.2023.282898. doi:10.3324/haematol.2023.282898
Sequential chemotherapy and lenalidomide followed by rituximab and lenalidomide maintenance for untreated mantle cell lymphoma. ClinicalTrials.gov. Updated February 21, 2023. Accessed October 13, 2023. https://tinyurl.com/39k5pde4