Progress in Prostate Cancer Care: Highlights From a Decade of Innovation
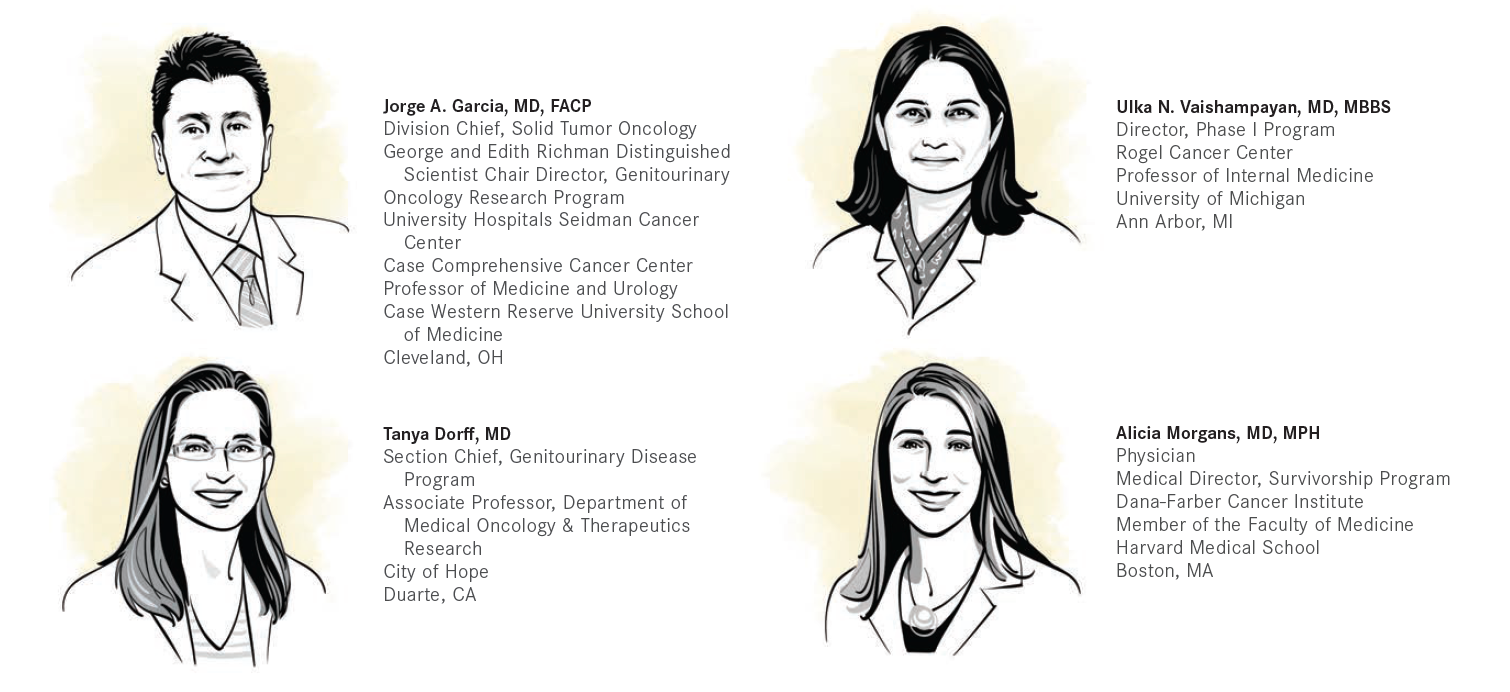
Targeted Therapies in Oncology asked some experts in prostate cancer diagnostics and therapeutics for their thoughts on the milestone improvements in treating patients with prostate cancer over the past decade.
There have been numerous changes to the standard of prostate cancer care in the past 10 years, with novel agents moving into earlier and different disease settings for prostate cancer and the introduction of radiopharmaceuticals into both the diagnostic and treatment spaces. Targeted Therapies in Oncology™ asked some experts in prostate cancer diagnostics and therapeutics for their thoughts on the milestone improvements in treating patients with prostate cancer over the past decade.
Shifting the Prostate Cancer Treatment Paradigm
The movement of regimens into new disease settings came from changing parameters of clinical trial design, according to Jorge A. Garcia, MD, FACP, chief of the Division of Solid Tumor Oncology, University Hospitals Seidman Cancer Center. “The bulk of the agents prior to 2012 were developed in the castration-resistant space in the postchemotherapy setting. So that was the paradigm of the time,” he said. “What became evident [was that] it was not necessary for us to wait that long, that we could consider giving these treatments earlier in the natural history of prostate cancer to see if we could [secure] a different outcome. I think the changes that you have seen since 2012 [include] the recognition that there may be a surrogate marker for outcome improvement so you don’t have to wait for a true survival end point but rather you can approve agents with radiographic progression-free survival improvement. We recognize that metastasis-free survival was a surrogate marker for outcomes for those patients in whom you have castration-resistant disease but you still didn’t see evidence of metastasis, and that led to the approval of agents such as apalutamide [Erleada], darolutamide [Nubeqa], and enzalutamide [Xtandi] in the N0 CRPC [nonmetastatic castration-resistant prostate cancer] space.”
That movement of therapies into earlier spaces was a notable advancement in treatments for prostate cancer, noted Ulka Vaishampayan, MD, MBBS, professor of internal medicine and director of the Phase 1 Program at the University of Michigan Rogel Cancer Center. Over the decade’s course, Vaishampayan said, “effective treatments were moved into earlier disease settings, so you don’t [have to] wait until patients with advanced prostate cancer. have progressed on hormone therapy.
Tanya Dorff, MD, section chief of the Genitourinary Disease Program at City of Hope, also views the movement of therapies into earlier lines of therapy as a major development in the past decade. “One of the biggest stories has been not just the new agents, which of course are very important, but how we’ve learned to optimize use of our existing agents. A huge story has been the movement of castration-resistant life-extending therapies up. front. to the hormone-sensitive setting where it seems [as though] their benefits are amplified. Just using the same drugs better has been quite a signifi cant advance for patients,” Dorff said.
Alicia Morgans, MD, MPH, genitourinary medical oncologist and the medical director of the Survivorship Program at Dana-Farber Cancer Institute, noted that 2012 heralded the start for many new options in the metastatic CRPC (mCRPC) space. “Before 2012, we had few options for therapy beyond androgen deprivation therapy [ADT] and docetaxel..Between 2010 and 2012 we saw the first approvals for treatments. beyond ADT, and they gradually worked their way into practice over the subsequent years. In 2012, we saw the approval of abiraterone [Zytiga] and enzalutamide in the postchemotherapy patient population [TIMELINE],. and these drugs absolutely transformed our ability to treat patients with very advanced mCRPC. The initial studies that led to these drugs being approved were performed in the postdocetaxel treatment space and gave an opportunity for patients who were at the end of the line, after they had.been through chemotherapy. Within a very short period of years [2013-2014], we gained.additional data that suggested that we could use abiraterone and enzalutamide before docetaxel chemotherapy, and that also gave us an opportunity to treat our patients who were not going to be eligible to get chemotherapy because they were too sick or too frail with something that might help prolong their life and maintain their quality of life [QOL].”1-4
Genomics
A significant portion of new treatments developed for prostate cancer occurred in concert with that of genomics, which has helped to improve prognostication and permitted the use of targeted therapies. “I think the homologous recombination repair mutations are important in prostate cancer because BRCA2 in particular appears to be associated with a more aggressive, poor prognosis prostate cancer diagnosis,5 and it is also something that can identify an individual who may have family members who are also at risk of other cancers within the heritable cancer syndrome associated with BRCA1 and BRCA2.6 This particular biomarker is also an opportunity for us to use targeted therapies [such as] PARP inhibitors to have better disease control, providing a new option for treating our patients,” Morgans said.
Garcia also noted the importance of biomarkers on the evolution of prostate cancer management. “Genomics are critically relevant to our patients, not only for us to be able to counsel patients properly, but to find a mutational change of relevance to them and their family members,” he said. “Genomics is equally important because now it becomes a therapeutic option for our patients. [Approximately] 10% of patients or so may have DNA repair defi ciencies and may therefore be candidates for PARP inhibitors, which are now FDA approved for that specifi c patient population.7,8 The NCCN [National Comprehensive Cancer Network] guidelines have changed drastically, and every man with advanced prostate cancer now undergoes genomic testing.”9
PARP inhibitors olaparib (Lynparza) and rucaparib (Rubraca) were approved by the FDA for prostate cancer within 4 days of each other. Rucaparib was first granted an accelerated approval on May 15, 2020, for the treatment of patients with deleterious BRCA mutation–associated mCRPC who have been treated with androgen receptor (AR)–directed therapy and a taxane-based chemotherapy.10 Then olaparib was approved on May 19, 2020, for the treatment of adult patients with deleterious or suspected deleterious homologous recombination repair gene–mutated mCRPC who have progressed following treatment with enzalutamide or abiraterone.11
Rucaparib was approved based on findings from the phase 2 TRITON2 trial (NCT02952534), which showed an objective response rate of 43.5% by independent radiology review and 50.8% by investigator assessment.10 Findings from the randomized phase 3 PROfound trial (NCT02987543) led to the approval of olaparib, with a median progression-free survival (PFS) of 7.4 months for the PARP inhibitor compared with 3.6 months with either enzalutamide or abiraterone in patients with an alteration in BRCA1, BRCA2, or ATM (HR, 0.34; 95% CI, 0.25-0.47; P < .001). The median overall survival (OS) was 18.5 months with olaparib vs 15.1 months in the control group (HR, 0.64; 95% CI, 0.43-0.97; P = .02).11
Immunotherapy in Prostate Cancer
Although targeted therapies have provided effective additions to prostate cancer management over the past decade, immunotherapy use in managing prostate cancer has been less encouraging. “It is clear that immune checkpoint inhibitors [ICIs] are quite active across a spectrum of cancers,” Garcia said. “But ICIs have not turned out to be drastically effective for patients with advanced prostate cancer.”12
When asked about these immunotherapy shortcomings, Dorff explained, “Immunotherapy has defi nitely been challenging in prostate cancer, and we’ve learned a lot about why that is. We know that the tumor microenvironment [TME] in prostate cancer is very hostile to the immune system.13 There are a lot of suppressive components of the immune system that are present in the tumor, so even if we can get T cells engaged, they may not be able to function once they arrive. Our 1 approved immunotherapy for prostate cancer is sipuleucel- T [Provenge],.which is an autologous activated cellular immunotherapy. The immune cells are activated ex vivo, and that’s the only one that’s ever prolonged survival.14 Although it doesn’t induce a lot of immediate objective responses or PSA [prostate-specific antigen] declines, there have been published case reports of complete responses.15 So they’re rare, but it speaks to the fact that this kind of cellular approach.may be something to pursue further with T-cell therapies, potentially if the.ex vivo activation.helps overcome the TME.”13
Sipuleucel-T was approved by the FDA in April 2010 for the treatment of patients with mCRPC who have asymptomatic disease and no visceral metastases. The approval was based on findings from the phase 3 IMPACT trial (NCT00065442), which randomly assigned patients with mCRPC to either sipuleucel-T or placebo. Median OS with the immunotherapy was 25.8 months compared with 21.7 months with placebo (HR, 0.78; 95% CI, 0.61-0.98; P = .03). At 36 months, the OS rate was 31.7% with sipuleucel-T and 23.0% with placebo.14
Radiopharmaceuticals
Other therapeutic modalities have generated more enthusiasm among the prostate cancer community. “With regards to therapeutics, clearly the biggest advancement was the introduction of therapeutic radiopharmaceuticals. Using radiation to treat cancer is not a novel concept. However, within prostate cancer, we’ve relied on EBRT [external beam radiation therapy]. The FDA approval of radium-223 [Xofi go] [in 2013], was a breakthrough moment for prostate cancer because you had much better radiopharmaceutical therapies, that actually improved OS,”14 said Phillip J. Koo, MD, chief of diagnostic imaging and oncology physician executive at the Banner MD Anderson Cancer.Center in Gilbert, Arizona. “Its effect on bone pain is variable, and we should focus on the fact it helps patients live longer. [It is] very exciting to see the adoption and integration of that into our practice guidelines and into our practices.” In the phase 3 ALSYMPCA trial (NCT00699751), radium-223 demonstrated an improvement in OS over placebo of 14.9 months vs 11.3 months in patients with CRPC and bone metastases (HR, 0.70; 95% CI, 0.58-0.83; P < .001).16
Prostate-specific membrane antigen (PSMA) has driven the more recent radiopharmaceutical and theranostic developments in prostate cancer.“ PSMA changes in response to different treatments and over the course of disease progression, being. up-regulated or down-regulated. in response to. exposure to different treatments. or expression of mutations that occur during disease evolution,” Morgans said. “It may be something that we can affect with our treatments, which is exciting, and it is something that we can target with. newer. treatment. approaches. In particular, 177Lu-PSMA-617 [Pluvicto], an approved agent for patients with mCRPC after progression of disease on docetaxel chemotherapy and AR-targeted agents, is something that we can already use in clinic to. treat patients..We. identify patients using a PSMA PET scan, which gives us some confidence that they will have a response to treatment. Lutetium is the first. of these PSMA-targeted approaches, but hopefully there will be.additional radiopharmaceuticals, small molecules, cellular-based therapies, and other treatments that target PSMA.”
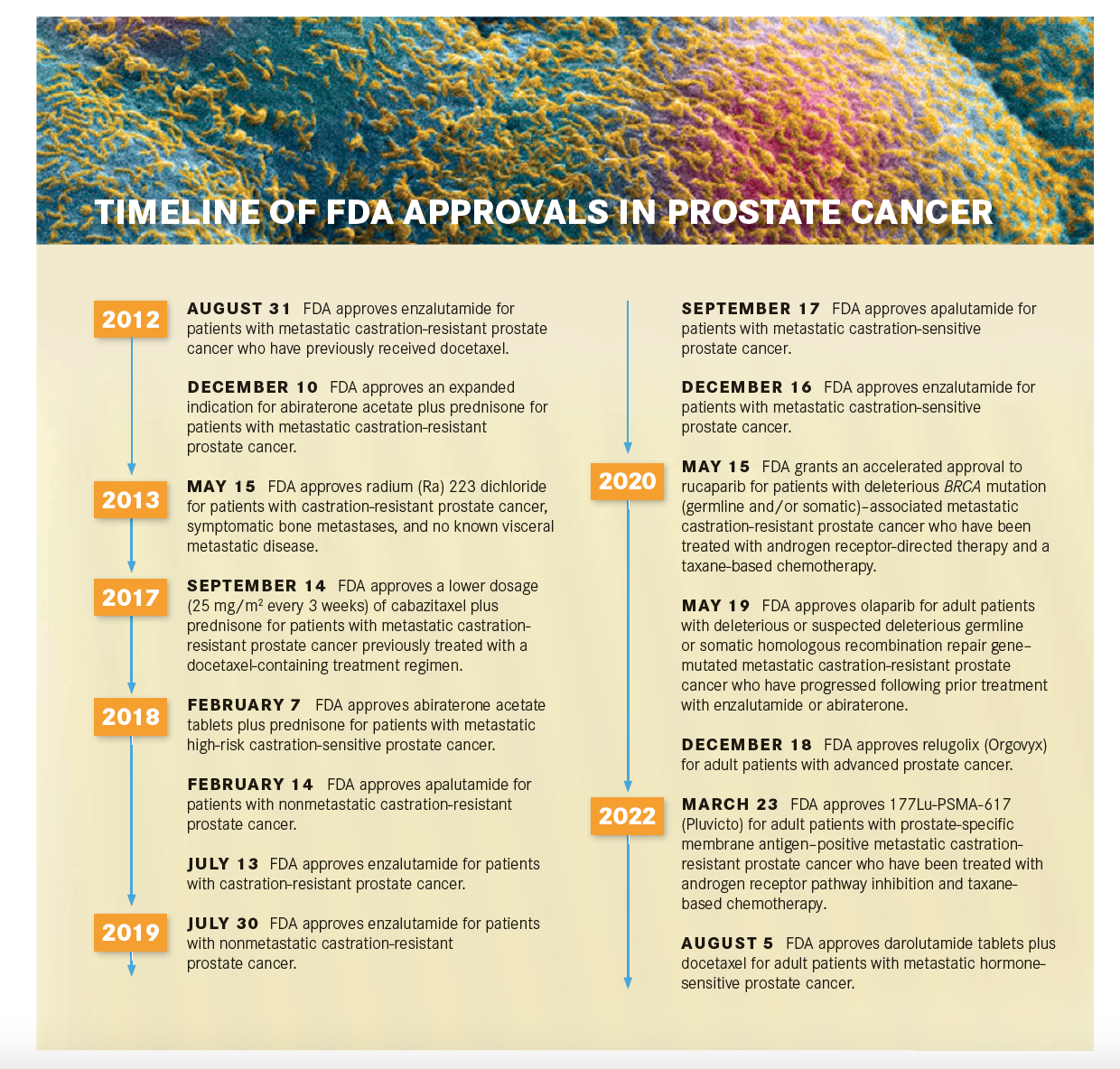
Koo also expressed enthusiasm for the use of PSMA in prostate cancer. “The biggest breakthrough on the diagnostic side came in the past couple of years when some of the PSMA-targeted diagnostic radiopharmaceuticals were FDA approved and then [made] commercially available throughout the United States,” Koo said. In the past year specifically, “the big highlight has been the approval of 177Lu-PSMA-617, being able to target the PSMA and get that OS benefit. The eagerly awaited results from phase 3 VISION trial [NCT03511664] were groundbreaking,” Koo said.17
VISION enrolled patients with mCRPC who were previously treated with an AR pathway inhibitor and 1 to 2 taxane treatments and were PSMA-positive by gallium- 68–labeled PSMA-11 PET-CT scans. They were randomly assigned 2:1 to receive either 177Lu-PSMA-617 plus standard of care or standard of care alone. Both PFS and OS were significantly improved with the addition of the radioligand therapy. At a median follow-up of 20.9 months, the median PFS was 8.7 months with 177Lu-PSMA-617 vs 3.4 months with standard therapy (HR, 0.40; 99.2% CI, 0.29-0.57; P < .001) and the median OS was 15.3 months and 11.3 months, respectively (HR, 0.62; 95% CI, 0.52-0.74; P < .001).17
Continued Research in Prostate Cancer
Therapeutic developments over the past decade are proof of the importance of ongoing research. “I continue to believe that the No. 1 priority for patients with prostate cancer is clinical trials,” Garcia said. “The only way for us to delay mortality, delay progression, and control disease effectively while we maintain QOL is to develop a sequence of evidence and a sequence of goals with the patient and their family to ensure that we don’t overtreat those who don’t need to be overtreated or to undertreat those who need more treatment.”
Dorff also spoke about the importance of clinical trials. “Some of the most exciting options for a patient who is progressing on first-line therapy are going be in clinical trials because we’re taking existing drugs and using them in combinations, for instance, or adding something new to an existingdrug to see if it’ll work better. So clinical trials can be the best bet as second-line. therapy or even first-line therapy, and not just after.all approved treatments have failed,” Dorff said.
In addition to clinical trial enrollment, Vaishampayan pointed to the importance of enrolling a more diverse clinical trial population. “The majority of the large, randomized clinical trials have had minimal enrollment and inclusion of diverse patient populations,” Vaishampayan said. “[In] our study…we enrolled a cohort of 40% African American patients with advanced prostate cancer. The results showed that intensifying treatment with the combination of ADT and enzalutamide up front in metastatic hormone-sensitive prostate cancer is critically important for the African American population because African American [patients] had an overall shorter survival if you just used ADT compared with [White] Americans. However, when we added an AR inhibitor—enzalutamide—to the ADT, both groups had comparable survival outcomes. This highlights the importance of studies across diverse populations.”18
The Bigger Picture for Prostate Cancer Care
Other aspects of care for patients with prostate cancer have become a focus in the past decade. “I think over the past 10 years, we have brought topics to the forefront of our conversation that are important not just to the scientists who investigate prostate cancer or the physicians who treat patients with prostate cancer every day but [also] are important to the patients themselves,” Morgans said.
“I think that we are trying to have conversations about how we optimize a patient’s QOL outside of the clinic as well and ensuring the treatments that we give treat the patient well, not just [manage] the disease effectively. And from a patient’s perspective, there’s nothing more important than having quality of time, not just time, at the end of the day. These initiatives to understand not only how we can treat prostate cancer but [also how to] take care of the human being are of critical importance,” Morgans said
REFERENCES:
1. Antonarakis ES, Eisenberger MA. Expanding treatment options for metastatic prostate cancer. N Engl J Med. 2011;364(21):2055-2058. doi:10.1056/NEJMe1102758
2. de Bono JS, Logothetis CJ, Molina A, et al; COU-AA-301 Investigators. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364(21):1995-2005. doi:10.1056/NEJMoa1014618
3. Scher HI, Fizazi K, Saad F, et al; AFFIRM Investigators. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367(13):1187-1197. doi:10.1056/NEJMoa1207506
4. Mohler JL, Armstrong AJ, Bahnson RR, et al. Prostate cancer, version 3.2012: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2012;10(9):1081-1087. doi:10.6004/jnccn.2012.0114
5. Narod SA, Neuhausen S, Vichodez G, et al. Rapid progression of prostate cancer in men with a BRCA2 mutation. Br J Cancer. 2008;99(2):371-374. doi:10.1038/sj.bjc.6604453
6. Pilarski R. The role of BRCA testing in hereditary pancreatic and prostate cancer families. Am Soc Clin Oncol Educ Book. 2019;39:79- 86. doi:10.1200/EDBK_238977
7. Abida W, Patnaik A, Campbell D, et al; TRITON2 investigators. Rucaparib in men with metastatic castration-resistant prostate cancer harboring a BRCA1 or BRCA2 gene alteration. J Clin Oncol. 2020;38(32):3763-3772. doi:10.1200/JCO.20.01035
8. de Bono J, Mateo J, Fizazi K, et al. Olaparib for metastatic castration- resistant prostate cancer. N Engl J Med. 2020;382(22):2091-2102. doi:10.1056/NEJMoa1911440
9. NCCN. Clinical Practice Guidelines in Oncology. Prostate cancer, version 4.2022. Accessed August 10, 2022. https://bit.ly/3Rb02D3
10. FDA grants accelerated approval to rucaparib for BRCA-mutated metastatic castration-resistant prostate cancer. FDA. May 15, 2020. Accessed August 12, 2022. https://bit.ly/3w4pySz
11. FDA approves olaparib for HRR gene-mutated metastatic castration- resistant prostate cancer. FDA. Updated May 20, 2020. Accessed August 12, 2022. https://bit.ly/3dBT7ED
12. Cha HR, Lee JH, Ponnazhagan S. Revisiting immunotherapy: a focus on prostate cancer. Cancer Res. 2020;80(8):1615-1623. doi:10.1158/0008-5472.CAN-19-2948
13. Runcie KD, Dallos MC. Prostate cancer immunotherapy-fi nally in from the cold? Curr Oncol Rep. 2021;23(8):88. doi:10.1007/s11912- 021-01084-0
14. Kantoff PW, Higano CS, Shore ND, et al; IMPACT Study Investigators. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411-422. doi:10.1056/NEJMoa1001294
15. Graff JN, Drake CG, Beer TM. Complete biochemical (prostate-specific antigen) response to sipuleucel-t with enzalutamide in castration-resistant prostate cancer: a case report with implications for future research. Urology. 2013;81(2):381-383. doi:10.1016/j.urology.2012.10.044
16. Parker C, Nilsson S, Heinrich D, et al; ALSYMPCA Investigators. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213-223. doi:10.1056/NEJMoa1213755
17. Sartor O, de Bono J, Chi KN, et al; VISION Investigators. Lutetium- 177-PSMA-617 for metastatic castration-resistant prostate cancer. N Engl J Med. 2021;385(12):1091-1103. doi:10.1056/NEJMoa2107322
18. Vaishampayan UN, Heilbrun LK, Monk P 3rd, et al. Clinical effi cacy of enzalutamide vs bicalutamide combined with androgen deprivation therapy in men with metastatic hormone-sensitive prostate cancer: a randomized clinical trial. JAMA Netw Open. 2021;4(1):e2034633. doi:10.1001/jamanetworkopen.2020.34633.

Bispecific Antibodies and ADCs Deliver a Futuristic Horizon Across Lung Cancer Settings
October 23rd 2024Recent advancements in protein engineering, especially antibody-drug conjugates, show promise in lung cancer treatment, with ivonescimab outperforming pembrolizumab in PD-L1-positive advanced non-small cell lung cancer.
Read More