Roundtable Discussion: Carraway Assesses Remaining Challenges in BPDCN Patient Population
During a Targeted Oncology™ Case-Based Roundtable™ event, Hetty E. Carraway, MD, MBA, discussed with participants diagnosing and treating patients with BPDCN, as well as the remaining challenges in this space.
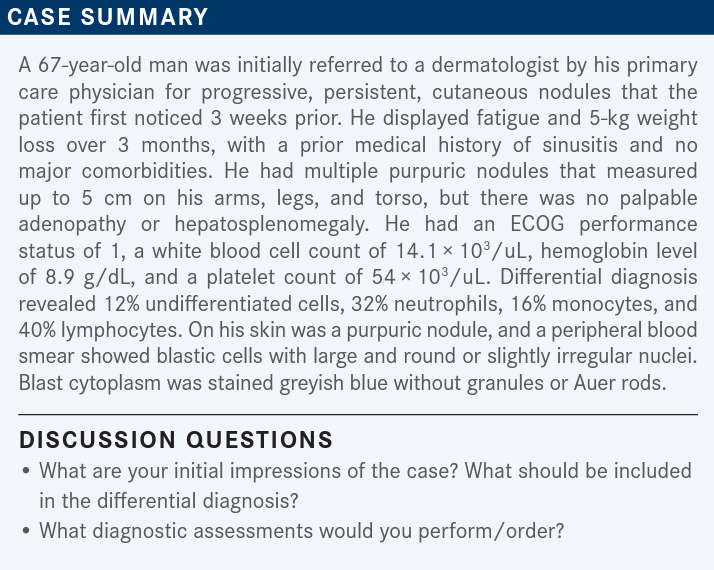
BABU: If a patient walks into the clinic and has skin nodules, pancytopenia, and cells that look like blasts, I would be concerned about acute myeloid leukemia [AML] or leukemia cutis, at least for a differential. But it [would] not be my differential unless the pathologist guided me in that direction.
CARRAWAY: I agree with your initial thoughts of AML and leukemia cutis. [Does anyone have] other thoughts?
MORRISON: It would be helpful to have flow cytometry on the blood sample to see what you have. The [patient] is going to need a bone marrow biopsy, too.
CARRAWAY: [We’re] already talking about what other assessments [we] would want to perform to get a better sense of what exactly is going on. Certainly, if you’re thinking about AML, as Dr Babu just shared, [the] next steps would be a bone marrow biopsy and flow cytometry. [Are there] any other laboratory tests you might want to use? Other differential diagnoses may include something like peripheral T-cell lymphoma or lymphoma rather than AML. [Would] anybody order an LDH [lactate dehydrogenase] test?
BABU: Yes, I think the normal panels for AML and acute lymphocytic leukemia are all pretty much the same, so I think we would all order that.
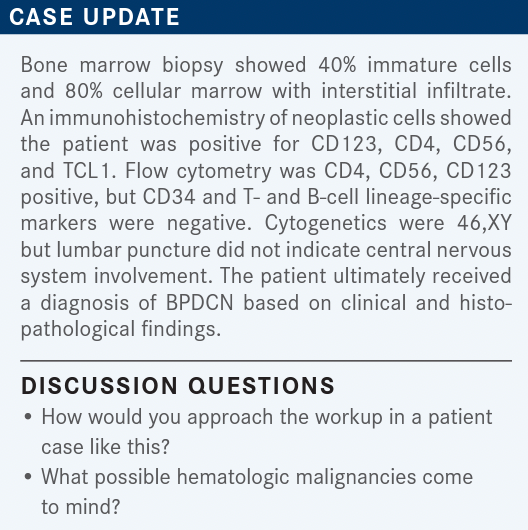
CHOWDHARY: Whenever possible, the skin biopsy and a good pathologic analysis of the infiltrating cells are important. One needs good immunohistochemistry because you can also have a lot of reactive processes that give you these kinds of plasmacytoid dendritic cells. Like in chronic myeloid leukemia or chronic myelomonocytic leukemia [CMML], even these can cause these kind of reactive cells, but I think immunohistochemistry generally differentiates that. Some of these chronic myeloproliferative disorders would also be in the differential diagnoses. I think there are even some benign conditions where you can see these kinds of cells in the skin and where you’d still want to be able to differentiate that.
CARRAWAY: I think that’s true that CMML is in your differential. Sometimes even infections could potentially make cells look blastic, so that could still be it. This is a talk on oncology, so we’re a little biased when thinking [about what it could be]. It’s hard to be broad in the initial case when you know we’re in oncology. But certainly, HIV and other types of viral infections could also be reasonably on the differential.
If we’re worrying about an oncologic diagnosis, especially with blastic plasmacytoid dendritic cell neoplasm [BPDCN], we want to look at the LDH and consider doing a PET/CT scan and all those tests. But we wouldn’t be rushing to do that until we did the first steps that we’ve been walking through. Certainly, the initial things we brought up, the bone marrow biopsy, flow cytometry, and skin biopsy, then you may get next-generation sequencing testing done. We’re doing that for most of our patients with any kind of leukemia or lymphoma, mostly with the leukemia or myeloid neoplasm workup.
BABU: I’m assuming [that because] there are hematologic abnormalities, one would assess that part before sending out the patient for other differentials, right?
CARRAWAY: Yes, I agree with you. I think at some point, if BPDCN becomes something you’re worried about, you’re going to confirm before you send the patient to another specialist. At this juncture, I think it’s reasonable to clarify what’s really going on before [moving] forward. That’s what I hear you saying, Dr Babu.
BABU: Yes. I’m assuming the patient got to the hematologic oncology tests because some basic assessment had already been performed.
CARRAWAY: Yes.
BABU: These patients are not going to just walk into our offices because they have skin lesions, right?
CARRAWAY: Right, exactly.
MORRISON: One thing that was not mentioned in the differential was potential fungal infection. Occasionally, you can get disseminated cryptococcosis, for example, that can present with skin nodules. If you were getting your dermatologist to do an initial biopsy, it would make sense to also submit some of that to the microbiology laboratory for stains and culture.
CARRAWAY: That’s a great point. So [it could be] ecthyma gangrenosum, whether it’s fungal or pseudomonal, especially if patients have pancytopenia. [That’s a] really good comment there. Some of these lesions are scary. I start thinking about melanoma [for the black lesions]. I start worrying about those types of skin lesions.
BARAI: Is the etiology of pancytopenia myelophthisic there, and the infiltration of the marrow?
CARRAWAY: It can be but not always. It’s kind of fascinating. I’ve seen patients have issues with low counts, but it’s pretty much directly from the infiltration of BPDCN into the marrow. I think if you catch patients early enough—and I’ve seen enough earlier patients where they just have only skin involvement and no impact on their bone marrow at all. But with time, the disease will progress and enter the bone marrow space. One of the more recent patients I’ve had presented with skin lesions but had no issues regarding her counts, thankfully.
KANDRA: Is it possible for patients to have a negative bone marrow and no pancytopenia?
CARRAWAY: Yes, absolutely. I’ve had patients in my practice just have skin lesions that were positive for BPDCN, a normal complete blood count, and a bone marrow biopsy that shows no evidence of BPDCN.
KANDRA: How familiar are the pathologists with this diagnosis when they look at the skin biopsy?
CARRAWAY: I like this question a lot because it depends on where the patient is seen, the experience of the pathologist, and [whether] they make sure to include immunohistochemistry stains to rule out BPDCN. It’s variable. That’s one of the reasons to share and learn about this particular entity—to make sure it’s considered in the differential diagnoses for patients with skin lesions with, or even without, pancytopenia.
HADDAD: [Some things] I think of as differentials include sarcomas, lymphomas, and melanoma for black lesions, like you mentioned, [as well as] extramedullary involvement of acute leukemia. All these just cross my mind. Also, systemic mastocytosis and the related situations. All these can be there, but Langerhans-type involvement as well, which all require a pathologist who is well versed in these conditions.
CARRAWAY: I agree with acute leukemia, as well. I also appreciate the fungal and viral infections.
BARAI: I thought that the overall response rates were impressive, but I’m kind of disappointed [with] the duration of response [DOR] and median overall survival [OS].1,2 Would I try it? Yes, because there are no other better therapies. So yes, I will use it. I don’t know what else we can do to get a longer DOR.
CARRAWAY: Thank you for your honest answer. I think for this diagnosis, nobody is quite happy with the OS for these patients if they can’t go to transplant.
CHOWDHARY: Certainly, these patients are rare, and for any of these patients in our regional general hematologic oncology programs, we would kind of be coordinating their care with our leukemia and lymphoma service at the main campus. But my question is: It seems like this is a treatment that even we could initiate at our centers as well, but at what point do we even consider transplant, or after how many treatments? If you’re getting a complete or a partial response, do we go to transplant? Is that an up-front evaluation and discussion?
CARRAWAY: Yes, it is. We talked about [whether] we are going to send this patient to another health care professional. That was probably getting at sending them to transplant. If you knew the patient had BPDCN, they’re young, and you can get disease control, [then] yes, you want to refer them to transplant as quickly as possible because their remissions are not prolonged remissions. You must get transplant teed up and, as many of us know, it just takes a long time to get typing between insurance coverage and everything else to happen in an expeditious manner. In these patients—it’s interesting—you can do flow cytometry and diagnose this with your CD1, -2, -3, -4, -5, or -6. One can measure to a small degree whether there’s involvement or not, even by flow cytometry. So the flow cytometry does give you a high sensitivity in terms of disease control.
I do think we’re getting better at diagnosing it sooner and seeing less bone marrow involvement, but it depends on where your patient is and what kind of process it took them to get diagnosed. Once you diagnose these patients, if they’re young enough and transplant candidates, you want to get going on that from the beginning.
And you want to do a lumbar puncture to make sure you’ve treated the CNS [central nervous system] so that’s not something that progresses or changes the trajectory of the patient’s care.
CHOWDHARY: We did not talk about the standard AML induction regimens in this condition, because this is not a randomized study. [Because] I have no experience using induction regimens, how does that compare with this treatment?
CARRAWAY: You’re pointing out an important part to the New England Journal of Medicine paper, in that it was upfront and/or relapsed/refractory patients with BPDCN, and there wasn’t really a control arm of 7 plus 3–based therapy [such as] AML induction or even hyper-CVAD [cyclophosphamide, vincristine, doxorubicin, dexamethasone]–based therapy [From the Data1].
In general, when we’ve treated these patients, there has not been a randomized study where patients with BPDCN get [randomly assigned] to 7 plus 3, hyper-CVAD, and SL-401. Part of that is because it’s a rare disease. And if there are only 300 patients, to get that number of patients on a study, the numbers aren’t enough. It would take too long for us to answer that question. When patients were diagnosed, the historical data show that these patients progressed quickly. And if you can’t get them to transplant, they will succumb to their disease and progress.
So you’re correct, it was not a phase 3 randomized study, and we don’t have that data. There were not large cohorts of patients who were put onto a study with just 7 plus 3 or just hyper-CVAD. We’re now trying to get some data in that space with other things [such as] venetoclax [Venclexta] as well, but those data currently are not as accessible as this study, which was in the up-front setting.1,2 [Because of] the historical controls where we saw their median OS was closer to 6 months, that led the FDA to approve SL-401 as one of the up-front therapies for these patients.3
KUMAR: I see the workup includes a lumbar puncture [LP] for all patients at diagnosis and relapse. [However], if there is no CNS disease, is there any CNS prophylaxis that we give, or do we just treat them as if they have CNS disease?
CARRAWAY: I would do an LP at the time of their diagnosis and see [whether] there’s any CNS disease. If there is not, then they don’t need any further intrathecal [IT] chemotherapy. If they’ve relapsed, I would do an LP again and evaluate for disease. If there’s no disease, they don’t need subsequent IT chemotherapy. If there is disease, then we would treat them as we would for any patient with CNS disease—twice a week until they have clearance, then once a week for every week for 4 treatments, and then once a month moving forward.
REFERENCES
1. Pemmaraju N, Lane AA, Sweet KL, et al. Tagraxofusp in blastic [lasmacytoid dendritic-cell neoplasm. N Engl J Med. 2019;380(17):1628-1637. doi:10.1056/ NEJMoa1815105
2. Pemmaraju N, Sweet KL, Stein AS, et al. Long-term benefits of tagraxofusp for patients with blastic plasmacytoid dendritic cell neoplasm. J Clin Oncol. 2022;40(26):3032-3036. doi:10.1200/JCO.22.00034
3. FDA approves tagraxofusp-erzs for blastic plasmacytoid dendritic cell neoplasm. News release. FDA. Updated December 26, 2018. Accessed February 14, 2023. https://bit.ly/3XsfihU
CAR T and CRS Adverse Events Considered in Relapsed Multiple Myeloma
October 24th 2024During a Case-Based Roundtable® event, Saad Z. Usmani, MD, FACP, MBA, discussed CAR T-cell therapy as third-line therapy for a patient with relapsed/refractory multiple myeloma and relevance of the KarMMa-3 trial for their treatment.
Read More