Ruxolitinib Controls Symptoms for Patients With Myelofibrosis
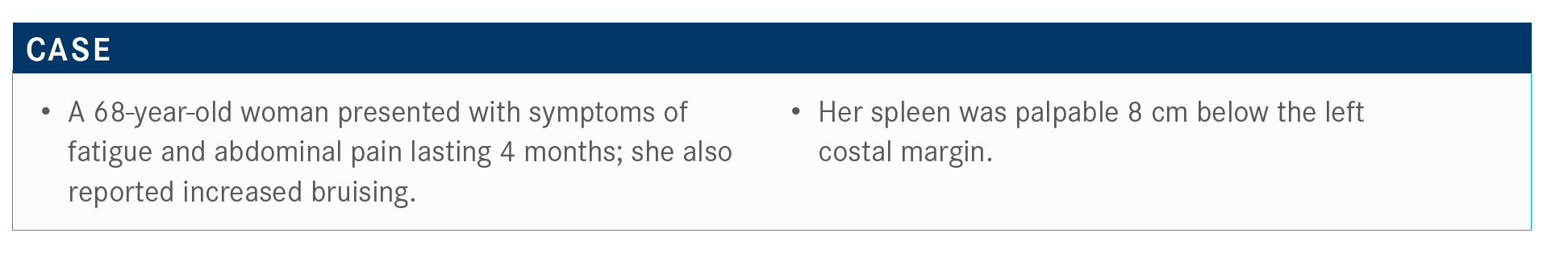
During a Targeted Oncology Case Based Peer Perspectives event, Rami Komrokji, MD, explored the use of ruxolitinib (Jakafi) for the treatment of a 68-year-old female patient with myelofibrosis.
Rami Komrokji, MD

During a Targeted Oncology Case Based Peer Perspectives event, Rami Komrokji, MD, senior member and professor of Oncologic Sciences, section head-Leukemia and Myelodysplastic Syndrome Vice Chair—Malignant Hematology Department, Moffitt Cancer Center, explored the use of ruxolitinib (Jakafi) in a 68-year-old female patient with myelofibrosis.
Targeted Oncology™: When you suspect myelofibrosis (MF) cases, how often do you perform a bone marrow biopsy on patients?
KOMROKJI: Not every fibrosis in the bone marrow is primary MF. I’ve had several patients with connective tissue diseases that have fibrosis in the bone marrow. I also had a couple of cases that were referred to me as MF but were lymphomas. One patient was set to go to transplant in a week for MF. He was young, in his 40s, and when our hematopathologists looked at the slides, they called me and said, “This looks like anything other than MF.” The patient had hairy cell leukemia with fibrosis in the bone marrow. With 1 week on cladribine [Mavenclad], he did very well.
Sometimes we get a lot of cases with large granular lymphocytic leukemia where you can see fibrosis in the bone marrow. The tough one for me is always to distinguish MF from myelodysplastic syndrome [MDS]/myeloproliferative neoplasms [MPNs] or MDS with fibrosis. The pathologists’ reports are a bit deceiving because the classical appearance of megakaryocytes in MPN is different dysplasia, and the description in the pathology report can look like they’re describing the megakaryocytes as dysplastic. [However,] they are really the classical cluster megakaryocytes we see in MPN. It depends on seeing more erythroid and megakaryocytic dysplasia.
Which tool do you use most often to access MF risk?
[When polled,] around a third [of oncologists] said they use the Mutation-Enhanced International Prognostic Score System [MIPSS70] or MIPSS70–plus. Most people probably use the Dynamic International Prognostic Scoring System [DIPSS]–plus, whereas others said they don’t use any formal assessment tool. There are about 5 or 6 staging systems for MF.
How does MF present itself in patients? How is it diagnosed?
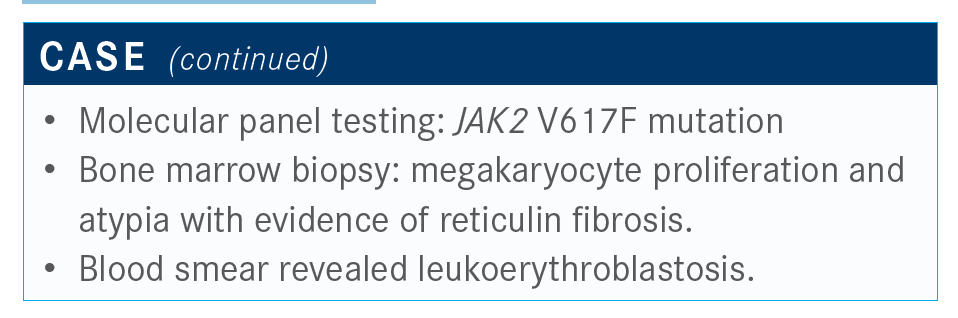
MF is not the most common myeloproliferative disease, but it’s the most symptomatic. Patients seem to present with hepatosplenomegaly, fatigue, and drenching night sweats. For diagnosis, major criteria need to be demonstrated [such as the] presence of fibrosis, although you could have prefibrotic MF, and presence of mutations, [like in genes such as] JAK2, CALR, or MPL. Minor criteria [includes] having anemia, splenomegaly, leukocytosis, leukoerythroblastosis, and [older] age.
The tricky [part of] diagnosis is either related to something that looks like MF or distinguishing it from MDS with fibrosis. We talk [a lot] about prefibrotic MF. Many of those patients are labeled as essential thrombocythemia [ET], but there are some slight differences if you look at the bone marrow. You need an experienced pathologist [because] the clustering of the megakaryocytes is different. You [can] see hyperplasia on the bone marrow in prefibrotic MF. We don’t treat prefibrotic MF differently from ET. In patients with prefibrotic MF, the rate of transformation to MF or acute myeloid leukemia is much higher. [For instance], patients who were labeled ET and in 2 years have leukemia or MF were probably prefibrotic MF.
There are also clinical-based [tools] discussed earlier, [such as] the IPSS, the DIPSS, or the DIPSS-plus. The idea [is] looking at patients’ symptoms—anemia, circulating blasts, white blood cell counts, [sometimes] karyotype—and then you can put the patients into a risk group. Like many diseases we deal with, MF is heterogeneous. We have patients with a median survival [exceeding] 10 to 15 years, and then some patients’ median survival will be less than a year.
The MIPSS70 and MIPSS70-plus are probably the most comprehensive. The MIPSS70 or MIPSS70-plus takes age out of the equation, so you still have the clinical variables. For the first time, they started looking at the degree or the extent of fibrosis as important. [In addition] to the phenotype driver mutations—CALR, JAK2, or MPL—having CALR is good, whereas the others are not. The absence of CALR is not good, particularly type 1. Then there are high-risk mutations: ASXL1, EZH2, SRSF2, andIDH1/IDH2, and U2AF1. Having 2 or more mutations matters.1,2
The patient is then placed in categories of very low to very high risk. [For instance], it’s probably OK to observe someone who has a median survival of 15 years and is low risk. [But] someone with a median survival of less than a year should be considered for a transplant.
To make it more complicated, there is a special model [myelofibrosis secondary to PV and ET prognostic model (MYSEC-PM)] if patients are secondary MF. Because almost half the patients we see as MF tend to be at the end stage of ET, cytopenias, blasts, mutations, and presence of symptoms will always [help] estimate the disease risk.3
What do the National Comprehensive Cancer Network [NCCN] guidelines look like for MF?
The NCCN guidelines had been in place for only a couple of years when they fi nally got guidelines for MPNs. It states that any model can be used and [breaks down] the models [by what it calls] lower risk versus higher risk. For example, if [a person’s score] is 4 or more using the MIPSS70-plus version 2.0, that’s a higher risk. Sometimes there is a discrepancy between [molecular and clinical] models, and typically, the molecular models win over the clinical models.4
How do you choose the type of JAK inhibitor therapy for patients?
Ruxolitinib for MF has been [FDA] approved for a while. Two studies have been done for ruxolitinib in MF—COMFORT-I [NCT00952289] and COMFORT-II [NCT00934544]. COMFORT-I was conducted in the United States against a placebo, [whereas] COMFORT-II was done in Europe against the best available therapy that included mostly supportive care or hydroxycarbamide.5,6
Those 2 papers showed around 30% to 40% spleen responses and almost 50% or more improvement. The primary end point is set as spleen volume reduction by 35%.5,6 Our studies require MRI. This is historically correlated with 50% [spleen volume] reduction by physical exam. So, the FDA adopted this as an objective assessment. But, in reality, the clinical benefit for many patients extends beyond that. That’s the least objective way of assessing the response.
What’s a meaningful reduction in the spleen?
I usually go by symptom relief; [basically,] if the patient could not tie their shoes before because of a big spleen, had ascites that [required] paracentesis, or had severe narcotic-requiring pain that stopped, even if they didn’t meet that reduction. We typically don’t repeat imaging studies. We go by physical exam or, at most, maybe an ultrasound.
Patients feel much better if JAK2 inhibitors [are used]. It’s an anti-inflammatory drug, so bone pain, night sweats, and itching go away quickly. [However] spleen response takes time; [typically,] 3 to 4 months. Symptom improvement happens within 1 to 2 weeks. If JAK2 inhibitors are stopped, symptoms come back quickly.
What does survival look like with ruxolitinib and how often is it used as first-line therapy?
[Because COMFORT-I and COMFORT-II] allowed crossover, it was a retrospective analysis examining survival. Even with crossover, there was a survival advantage with ruxolitinib over placebo. Compared with [hydroxycarbamide] or the best available therapy, patients had a survival advantage [with ruxolitinib].5,6 I present this to patients, because I would not stop ruxolitinib treatment to improve their survival. It doesn’t improve survival if patients are asymptomatic. [However,] a patient who fits the intermediate or high-risk group with constitutional symptoms and splenomegaly will derive a survival advantage from [this drug].
There is some correlation for patients with spleen reduction at 6 months and durable spleen reduction, that they derive survival advantage. At [The University of Texas] MD Anderson [Cancer Center], the MPN group is aggressive on starting the patients on the highest dose [of ruxolitinib], even if they make the patient become transfusion dependent. They believe that if you reduce the spleen [size] and the patient’s symptoms get better early on, then there’s more survival advantage. Some other [cancer centers] worry more about pushing [a high] dose from the beginning. At Moffitt Cancer Center, we are somewhere in between. We sometimes start at a lower dose if a patient’s [blood] counts are borderline, but then we quickly escalate if they tolerate the treatment to try to achieve a spleen response.
If [the goal] is to target constitutional symptoms [like] fatigue, drenching night sweats, or splenomegaly, then ruxolitinib [should be] used. Don’t use ruxolitinib if you are [trying to target] cytopenias, and for someone who] is anemic or thrombocytopenic, [this treatment] will make it worse. The toughest groups [to treat] are patients with big spleens, constitutional symptoms, and anemia. Some patients will [be fine], but for others, the cytopenia would be worse.
Symptom improvement happens at the dose of 5 or 10 mg of ruxolitinib, whereas spleen response is dose dependent. You rarely will see the spleen shrinking down on 5 mg of ruxolitinib.
How does taking a patient off of ruxolitinib work?
If [patients] are responding, you don’t want to take them off immediately, because their symptoms will come back. There have been reports of [reactions similar to] withdrawal when stopping the JAK2 inhibitors. Patients can become sick, [and we] try to prevent a cytokine storm for those patients.
If a patient is progressing on ruxolitinib and their symptoms are back, I’m not sure there is value in using ruxolitinib—the same [goes] for a transplant. We continue them on ruxolitinib until day 0 of the transplant. Then we start tapering them, and sometimes they continue [treatment] even after transplant because ruxolitinib is now used for graft-vs-host disease.
What types of toxicities are seen with ruxolitinib?
Anemia and thrombocytopenia [are the most common adverse events], and [patients are] less likely to see neutropenia. The hemoglobin will drop almost expectedly by 2 g by week 8.5,6 When we start [treatment], we bring patients in every 1 to 2 [months]. That’s when I sometimes escalate the dose. If they develop profound cytopenia, we back off or stop the treatment.
In patients with low platelet count, there was a study [EXPAND; NCT01665144] that looked at starting with lower doses of ruxolitinib. The maximum starting safe dose was identified to be 10 mg.7 Responses were seen in around 30% of the patients. [However], it’s not easy, particularly when the counts are low or the platelets are around the 50s. There was some symptom benefit because it’s a lower dose, but it’s hard to see the spleen response unless you push the dose. Once you go above the 10 mg, you will start seeing the spleen response in those patients.
With EXPAND, [patients were] divided into 2 groups [by platelet count], 50 to 74 and 75 to 100. Cytopenia was more profound within patients that had lower platelets [78%]. Later on, there was discontinuation in almost a third of the patients because of cytopenias.7
How does fedratinib (Inrebic) differ from ruxolitinib?
[Fedratinib] is an FLT3 inhibitor, whereas ruxolitinib is a JAK1/JAK2 inhibitor. Two trials were done, JAKARTA [NCT01437787] and JAKARTA2 [NCT01523171]. They were similar groups, intermediate-2 or high-risk [primary MF], that were randomized to 2 doses of the fedratinib versus placebo.8
Responses were around 36% seen with fedratinib in an up-front setting, and the symptom response was in the range of 30% to 40% based on the platelet count.
The toxicity profile [of fedratinib] is a bit different from ruxolitinib because it causes fewer cytopenias with anemia and thrombocytopenia. Although the numbers look similar to the COMFORT trials, the study allows patients with lower baseline blood counts to enroll. [However], there are more gastrointestinal toxicities. Anytime you have a medication that’s going to target FLT3, we will see some gastrointestinal toxicity, [such as] nausea, vomiting, and diarrhea.
JAKARTA looked at patients who were never treated with ruxolitinib compared with JAKARTA2 that looked at patients who were treated with ruxolitinib. [JAKARTA] helped define ruxolitinib failure, such as either cytopenias, intolerance, or failure of spleen response. So if patients on ruxolitinib [fail treatment], fedratinib could be a second-line option for those patients.
Are there other therapies in the pipeline?
Momelotinib, another JAK1/JAK2 inhibitor, is in development. It’s going into a phase 3 trial now. Hopefully, we will have the study open in November [at Moffitt]. Momelotinib was not as good at reducing the spleen, but it’s good for symptoms, and it’s the only JAK2 inhibitor that patients have seen anemia response.
Then there is pacritinib that has been in development for a long time. Pacritinib is also a JAK2 [inhibitor] and has FLT3 activity. Because of its nature, pacritinib, if it gets approved, is probably going to be for patients with thrombocytopenia or severe thrombocytopenia.
References:
1. Guglielmelli P, Lasho TL, Rotunno G, et al. MIPSS70: mutation-enhanced international prognostic score system for transplantation-age patients with primary fibrosis. J Clin Oncol. 2018;36(4):310-318. doi:10.1200/JCO.2017.76.4886
2. Tefferi A, Guglielmelli P, Lasho TL, et al. MIPSS70+ version 2.0: mutation and karotype-enhanced international prognostic scoring system for primary myelofibrosis. J Clin Oncol. 2018;36(17):1769-1770. doi:10.1200/JCO.2018.78.9867
3. Passamonti F, Alessandro V, Domenica C, et al. A new international multicenterbased model to predict survival in myelofibrosis secondary to polycythemia and thrombocythemia: the Mysec Prognostic Model (MYSEC-PM). Blood. 2014; 124(21):1826. doi:10.1182/blood.V142.21.1826.1826
4. NCCN. Clinical Practice Guidelines in Oncology. Myeloproliferative neoplasms; version 1.2020). Accessed May 21, 2020. https://bit.ly/2U6puyl
5. Verstovek S, Mesa RA, Gotlib J, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366(9):799-807. doi:10.1056/NEJMoa1110557
6. Harrison C, Kiladjian JJ, Al-Ali HK, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366(9):787-798. doi:10.1056/NEJMoa1110556
7. Vannucchi AM, Te Boekhorst PAW, Harrison CN, et al. EXPAND, a dose-finding study of ruxolitinib in patients with myelofibrosis and low platelet counts: 48-week follow-up analysis. Haematologica. 2019;104(5):947-954. doi:10.3324/haematol.2018.204602
8. Pardanani A, Harrison C, Cortes JE, et al. Safety and efficacy of fedratinib in patients with primary or secondary myelofibrosis: a randomized clinical trial. JAMA Oncol. 2015;1(5):643-651. doi:10.1001/jamaoncol.2015.1590

Bispecific Antibodies and ADCs Deliver a Futuristic Horizon Across Lung Cancer Settings
October 23rd 2024Recent advancements in protein engineering, especially antibody-drug conjugates, show promise in lung cancer treatment, with ivonescimab outperforming pembrolizumab in PD-L1-positive advanced non-small cell lung cancer.
Read More