Sborov Looks at Combination Therapies in Relapsed/Refractory Multiple Myeloma
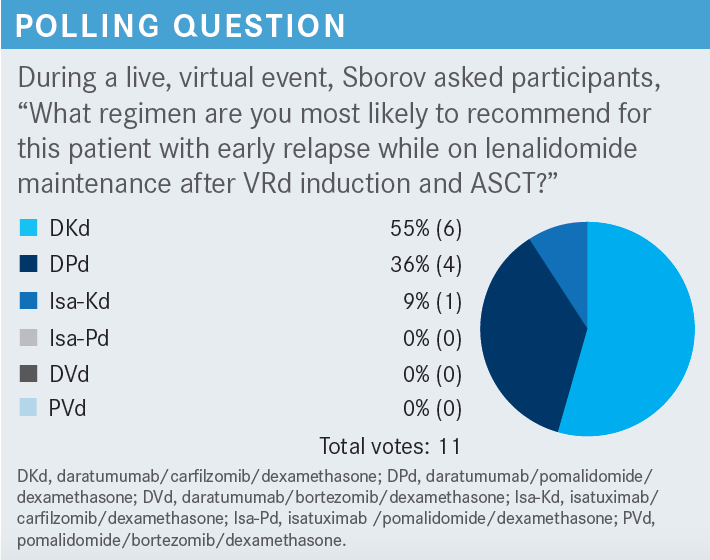
During a Targeted Oncology™ Case-Based Roundtable™ event, Douglas W. Sborov, MD, MS, discussed possible therapy options for a patient who relapsed after receiving bortezomib, lenalidomide, and dexamethasone followed by autologous stem cell transplant.
Douglas W. Sborov, MD, MS
Associate Professor, Division of Hematology and Hematologic Malignancies
Department of Internal Medicine
University of Utah School of Medicine
Director, Multiple Myeloma Program and Division of Hematology Biorepository
Huntsman Cancer Institute
Salt Lake City, UT

CASE SUMMARY
- A 60-year-old White woman received a diagnosis of Revised International Staging System stage II multiple myeloma.
- Fluorescence in situ hybridization cytogenetics: 1q21 (3 copies)
- ECOG Performance Status score: 0
- At the time, she was treated with bortezomib (Velcade), lenalidomide (Revlimid), and dexamethasone (VRd) induction therapy, followed by autologous stem cell transplant (ASCT).
- She achieved a complete response and minimal residual disease (MRD) negativity.
- The patient was placed on lenalidomide maintenance therapy for 2 years.
- On follow-up, the patient reported severe fatigue and pain in her back and legs that was impairing her ability to work full time.
- M protein level: 1.98 g/dL (rapid increase from prior blood work)
- λ free light chain level increased from 47.5 mg/dL to 136.7 mg/dL
- Hemoglobin level: 9.8 g/dL
- White blood cell count and platelets: within normal limits
- Creatinine level: 1.4 mg/dL (range, 0.59-1.04 mg/dL)
- Estimated glomerular filtration rate: 45 mL/min/1.73m2
- PET scan showed vertebral fracture at L1 and lesions in both femurs.
- ECOG Performance Status: 1
- A decision to switch therapy was made.
Targeted OncologyTM: Can you go over the National Comprehensive Cancer Network (NCCN) guidelines for relapsed/refractory multiple myeloma?
SBOROV: As hard as we try to make this easier for everybody in the community with the NCCN guidelines, I fear that we make it even more complicated. What we’ve done in the last year is [phrase it as] having patients who are bortezomib or carfilzomib [Kyprolis] refractory, or having patients who are lenalidomide refractory. The majority of our patients at this point are going on lenalidomide maintenance. The question is, is the patient progressing off… lenalidomide or are they progressing off…nothing, because a lot of times we are stopping lenalidomide maintenance. I am not seeing a whole lot of bortezomib maintenance in the community anymore, which I think is probably appropriate.1
[For patients who are bortezomib refractory], there is daratumumab [Darzalex]/lenalidomide/dexamethasone [DRd] based on the POLLUX trial [NCT02076009] for patients who are not lenalidomide refractory.2 There’s also daratumumab/ carfilzomib/dexamethasone [DKd] based on CANDOR [NCT03158688];3 carfilzomib/lenalidomide/dexamethasone [KRd] based on ASPIRE [NCT01080391];4 isatuximab [Sarclisa]/carfilzomib/dexamethasone [Isa-Kd] based on IKEMA [NCT03275285];5 and carfilzomib/pomalidomide [Pomalyst]/dexamethasone [KPd] based on phase 2 data.6
Then on the opposite side, [for patients who are lenalidomide refractory], we don’t want to use lenalidomide, so we are just going to pick our favorite triplet. I think it’s worthwhile to highlight that there are no doublets [in the guidelines].1 Doublets are a thing of the past. We are using triplets across the board. We’re not using Kd as a doublet in this population anymore either. We should be utilizing it in a triplet.
There are all sorts of data out there, so you could probably use some other regimens. I think that the [therapeutic] space at first relapse is becoming clearer. Then what happens is you have somebody who is progressing and they have had 2 prior lines of therapy.
So what do you do in that case, when you are not yet ready to go to a chimeric antigen receptor-T cell therapy, teclistamab [Tecvayli], or whatever else? What do you do in that space? I think that’s the big question. We wanted to make sure when we were writing the NCCN guidelines that physicians had all sorts of options that they could choose from. Basically, you want a triplet and you want to identify drugs that the patient has not seen yet after that second progression. This space is changing a lot, and I think we are going to see big-time changes in the next 2 or 3 years.
Can you briefly describe the previous treatments received in the phase 3 trials for relapsed/refractory multiple myeloma?
We always say you are not supposed to make cross-trial comparisons and I think this highlights why we should not. We have all…these different randomized phase 3 trials, and we can think about all these [treatment options] in patients with 1 to 3 prior lines of therapy.
For example, in POLLUX, for patients who had at least 1 prior line of therapy, 20% were refractory to proteasome inhibitor [PI] and 2.5% were refractory to lenalidomide and PI.2 They were not heavily pretreated patients and ultimately were not lenalidomide refractory. So in somebody who is not lenalidomide refractory, what do you go to? You should be going to DRd. That should be your decision for treatment after first progression.
Then CANDOR included patients with 1 to 3 prior lines of therapy.3 Thirty percent of the patients were lenalidomide refractory and 30% were bortezomib refractory. They didn’t report on how many patients were refractory to both.
Then IKEMA [patients] had 1 to 3 prior lines of therapy.5 A third were lenalidomide refractory, 30% were bortezomib refractory, and 20% were dual refractory.
Another important trial, APOLLO [NCT03180736], looked at daratumumab/pomalidomide/dexamethasone [DPd].7 Patients had 1 to 3 prior lines of therapy, but 80% of these patients were lenalidomide refractory. Almost 50% were PI refractory, and 40% were dual refractory.
So you can’t compare all…these trials because you are not looking at apples to apples, but I think it is still important to look at this group of data and try to tease it out a little bit.
What are the options for patients with 1 prior line of therapy?
The CASTOR [NCT02136134] trial looked at daratumumab/bortezomib/dexamethasone [DVd]. Median progression-free survival [PFS] with DVd was 16.7 months in not heavily pretreated patients.8 The OPTIMISMM [NCT01734928] trial looked at pomalidomide/bortezomib/dexamethasone [PVd] vs Vd.9 The PFS was 11.2 months with PVd. DVd and PVd are not my favorite regimens. In patients who don’t have aggressive relapse, you could maybe think about those regimens, but I think that we can do better.
For CANDOR, using DKd, median PFS was 28.6 months.3 [This was] a similar population to the IKEMA trial, which used Isa-Kd, and that median PFS was 41.7 months.5,10 This is something that’s new for most of us. Most of us [were thinking we] didn’t know that Isa-Kd was that good. One of the other regimens that we think about in patients who are lenalidomide refractory is DPd. In my opinion, DPd is still a very good regimen.
APOLLO, with more heavily pretreated patients, had a median PFS of 12.5 months in that population.7 But, when you look at the [POM] MM 014 trial [NCT01946477], which investigated DPd, [it] was a phase 2 trial.11 But these patients were much less heavily pretreated. For patients who were lenalidomide exposed but not refractory, their median PFS was 30.8 months.
For patients who were lenalidomide refractory, their median PFS was 2 years. So maybe not as good as a carfilzomib-based regimen, but when you are talking about that patient who doesn’t want to come in twice a week for carfilzomib, or may not want infusion, they want to just go on an oral agent and subcutaneous daratumumab, DPd can be a good regimen to consider.
CASE UPDATE
- PET/CT scan demonstrated new lytic lesions.
- The patient was started on Isa-Kd and achieved a very good partial response.
What was the design and efficacy of the IKEMA trial investigating Isa-Kd?
IKEMA was a randomized phase 3 trial.5,10 The primary end point was PFS. Three hundred patients were included with 1 to 3 prior lines of therapy, no prior carfilzomib, and not refractory to prior anti-CD38 antibody. The Isa-Kd regimen was given at 10 mg/kg. Isatuximab was given in an infusion, weekly for the first cycle and then every other week thereafter. Carfilzomib was given at 20 mg/m2 on days 1 and 2, and then at 56 mg/m2 thereafter on days 8, 9, 15, and 16 in cycle 1, and then on days 1, 2, 8, 9, 15, and 16 in all subsequent cycles. Kd was given per the same dosing.
Patient characteristics were well matched overall. This did include older patients, at least 10% in both arms. Twenty-three percent to 25% of the patients had high-risk cytogenetic features; 42% in each arm had gains of 1q21. We don’t tease out 3 vs 4 copies.
These are probably the most important data: the median PFS, based upon the FDA-mandated censoring rules, was 41.7 months with Isa-Kd vs 20.8 with Kd [HR, 0.59; 95% CI, 0.42-0.83].10 When you look at the original statistical design of the trial, the median PFS was about 3 years vs 19.2 months, respectively [HR, 0.58; 95% CI, 0.42-0.79].
But I think keying in on this 41.7 months is important, especially when we look at DKd, for which the median PFS was about 29 months.3 So if I’m thinking about using carfilzomib in this setting, at least based on these data, I’ve switched my practice to utilizing isatuximab, primarily because I am avoiding that problem of the infusion vs subcutaneous [administration]. In all the subgroup analyses, we saw that the triplet therapy was favored over the doublet, which is not surprising given everything we know.10 I’d highlight that Isa-Kd was beneficial in patients with renal insufficiency as well as 1q21, which is why we picked it for this case.
For depth of response in patients treated with the triplet, 44% of patients had complete response or better, and 34% of the patients were MRD negative compared with 15% with Kd [OR, 2.09; 95% CI, 1.26-3.48]. Those patients, at first progression or after first progression, can still get deep responses, and a third of them are getting into MRD negativity.
Utilizing the triplet prolonged the time to next treatment, at 45 vs 25 months [HR, 0.55; 95% CI, 0.40-0.76]. Overall survival has not been reached with 44 months of follow-up. This is not surprising, but we will see these data mature.
How did patients do in terms of toxicity in IKEMA?
I think it’s important to bring up the concept of what’s happening with the cardiac issues.10 It’s important to note that the addition of isatuximab did not increase cardiac toxicity. What’s driving those cardiac events is the carfilzomib. In addition, we would expect that the addition of an anti-CD38 antibody is going to increase rates of cytopenias as well as diarrhea, hypertension, fatigue, pneumonia, and other infections. Infusion reactions with isatuximab, just like daratumumab when we’re using it intravenously, happened mostly at the first or second dose, and primarily at the first dose. Primarily, these are grade 1 and 2 events, with very few grade 3 or higher events. About 40% of the patients are getting infusion reactions. So it really speaks to the importance of utilizing prophylactic medications, like we are doing with daratumumab.
REFERENCES
1. NCCN Clinical Practice Guidelines in Oncology. Multiple myeloma, version 3.2023. Accessed March 10, 2022. https://bit.ly/2T0mDYS
2. Dimopoulos MA, Oriol A, Nahi H, et al; POLLUX Investigators. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(14):1319-1331. doi:10.1056/NEJMoa1607751
3. Dimopoulos M, Quach H, Mateos MV, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): results from a randomised, multicentre, open-label, phase 3 study. Lancet. 2020;396(10245):186-197. doi:10.1016/S0140-6736(20)30734-0
4. Stewart AK, Rajkumar SV, Dimopoulous MA, et al; ASPIRE Investigators. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372(2):142-152. doi:10.1056/NEJMoa1411321
5. Moreau P, Dimopoulos MA, Mikhael J, et al; IKEMA study group. Isatuximab, carfilzomib, and dexamethasone in relapsed multiple myeloma (IKEMA): a multicentre, open-label, randomised phase 3 trial. Lancet. 2021;397(10292):2361- 2371. doi:10.1016/S0140-6736(21)00592-4
6. Sonneveld P, Zweegman S, Cavo M, et al. Carfilzomib, pomalidomide, and dexamethasone as second-line therapy for lenalidomide-refractory multiple myeloma. Hemasphere. 2022;6(10):e786. doi:10.1097/ hs9.0000000000000786
7. Dimopoulos MA, Terpos E, Boccadoro M, et al; APOLLO Trial Investigators. Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma (APOLLO): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(6):801-812. doi:10.1016/S1470-2045(21)00128-5
8. Palumbo A, Chanan-Khan A, Weisel K, et al; CASTOR Investigators. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(8):754-766. doi:10.1056/NEJMoa1606038
9. Richardson PG, Oriol A, Beksac M, et al; OPTIMISMM trial investigators. Pomalidomide, bortezomib, and dexamethasone for patients with relapsed or refractory multiple myeloma previously treated with lenalidomide (OPTIMISMM): a randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(6):781-794. doi:10.1016/S1470-2045(19)30152-4
10. Pektas O, Moreau P, Dimopoulos MA, et al. Updated progression-free survival (PFS) and depth of response in IKEMA, a randomized phase 3 trial of isatuximab, carfilzomib and dexamethasone (isa-KD) vs KD in relapsed multiple myeloma (MM). Hematol Transfus Cell Ther. 2022;44(suppl 1):S15. doi:10.1016/j.htct.2022.09.1211
11. Siegel DS, Schiller GJ, Samaras C, et al. Pomalidomide, dexamethasone, and daratumumab in relapsed refractory multiple myeloma after lenalidomide treatment. Leukemia. 2020;34(12):3286-3297. doi:10.1038/s41375-020-0813-1
