Trial Results Show Patients With RET Alterations Experience Different Efficacy With Lung Cancer Therapies
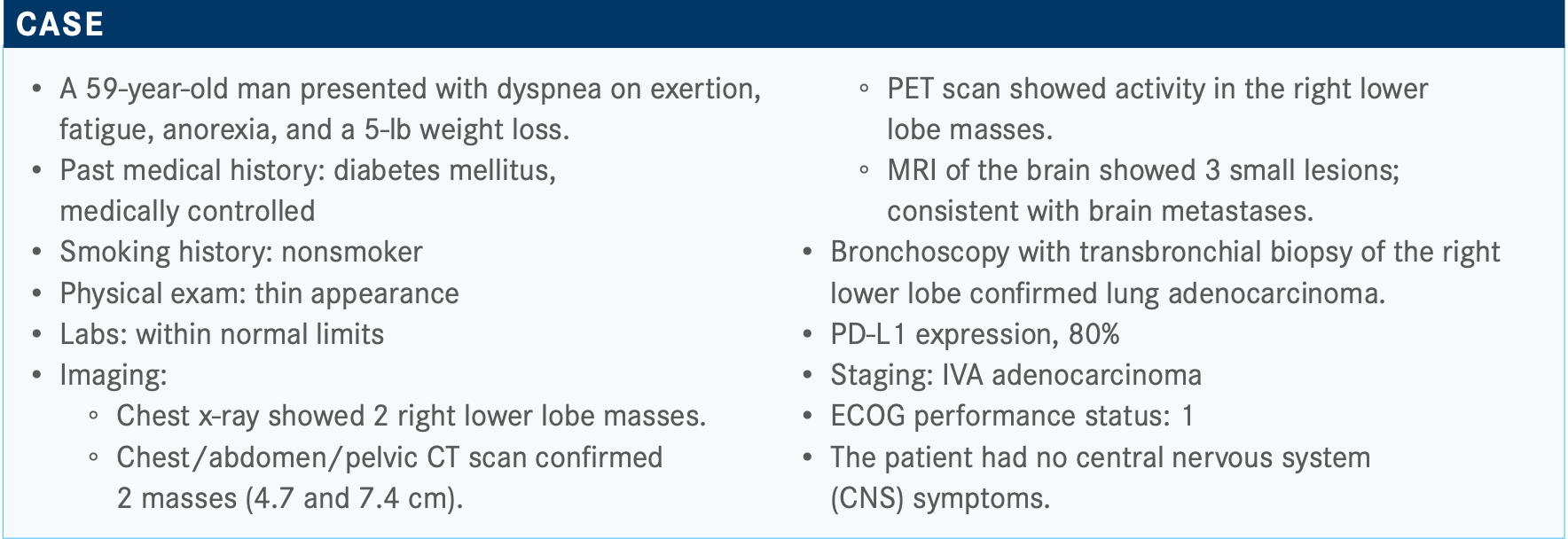
During a Targeted Oncology Case-Based Peer Perspectives event, Todd Bauer, MD, medical oncologist, Tennessee Oncology, discussed the results from clinical trials that include patients with RET-altered lung cancer to determine a treatment strategy for a 59-year-old patient.
Todd Bauer, MD

During a Targeted Oncology Case-Based Peer Perspectives event, Todd Bauer, MD, medical oncologist, Tennessee Oncology, discussed the results from clinical trials that include patients with RET-altered lung cancer to determine a treatment strategy for a 59-year-old patient.
Targeted OncologyTM: Do you tend to initiate therapy right away or wait to receive molecular testing results?
BAUER: There have been study results that showed that practitioners are less patient than patients to start treatment. If we have a good educated discussion with our patient and sit down and say, “Here are the reasons I think this is important for you to wait,” most patients, by and large, will wait. I think especially with the data about rates of post immunotherapy TKI [tyrosine kinase inhibitor] pneumonitis, I would have concern or want them to wait for [the molecular testing results].
We tend to think of these alterations as being rare, and indeed, some of them are. So, if you start with TRK—which is probably the lowest [frequency] at less than 1%, probably 0.1%, if we’re being honest, in lung [cancer]—ALK, ROS1, RET, EGFR, MET, you’re approaching 35% to 40% of patients who should have some alteration there. So, that’s saying, “Man, I have almost a coin flip of sparing you chemotherapy and immunotherapy and getting you on something you can take by mouth that can do better.” So I think that’s part of that discussion that we owe it to our patients to have.
How often do you find RET fusions in patients with lung adenocarcinoma?
RET occurs 2% to 3% of the time. It’s a lot like ROS1 in its frequency, which is also rare. This is why I reiterate that we have to test everyone for all of these, because you can’t go out just looking for those individual tests. You’re going to get frustrated and stop testing if you don’t look for everything.
RET [alterations do] occur in a number of different cancers, but what we know is that with medullary thyroid cancer, RET mutations are drivers, especially of familial medullary thyroid cancer but also over 60% of sporadic thyroid cancers.1 RET fusions [are found] in anaplastic thyroid cancer, papillary thyroid cancer, and other non–medullary thyroid cancers, [as well as] in lung acdenocarcinomas. This is again where the details matter. If you see a RET fusion in lung or nonmedullary thyroid cancer, that serves as a driver alteration and should be considered for targeting. If you see a RET mutation in a medullary thyroid cancer, that serves as a driver and should be considered for targeting. [I remember it by] medullary, mutated; everything else, fused. We also have not had good evidence that these alterations work as drivers in other types of cancers. So, right now, the approvals that we will talk about are just in adenocarcinoma of the lung with a RET fusion, medullary thyroid carcinoma with a RET mutation, and nonmedullary thyroid carcinoma with a RET fusion. So you see that they do come across in different frequencies.
Do you think that this patient scenario represents a typical case of RET-rearranged non–small cell lung cancer (NSCLC)?
The best example I have of this is a patient that Patrick Murphy, MD, sent me—a never smoker, business owner in Brentwood, who had some shoulder pain. They imaged it, and he had a lytic lesion in his right scapula. And then they did further imaging and had a lung lesion, and biopsy showed lung cancer. So [the patient was sent] for palliative radiation of the scapula. While we were waiting on these [results], he came back with a RET fusion, much like this patient, and he was started on up-front treatment with a RET inhibitor. So I think that’s an appropriate way to go.
How do you generally approach the management of baseline brain metastases in patients such as these?
A lot of these patients with RET-rearranged lung cancer, just like in our ALK-positive lung cancer population, are prone to develop brain metastases if they do not have them at diagnosis.
I think if we just have chemotherapy, that’s probably a reasonable option. But what we’re going to see is that these TKIs, much like we see in some of the ALK drugs, cross the blood-brain barrier well and can take effect quickly, typically at the time of first reimaging. So we may be able to spare patients those adverse effects [AEs] of radiation that they get even with SRS [stereotactic radiosurgery] over the course of a lifetime.
For patients with RET-rearranged, PD-L1–high, metastatic NSCLC, what systemic therapy options are available?
Selpercatinib [Retevmo] was previously known as LOXO-292. This is like one of my oldest children. I gave the first dose [of this drug] in a human about 4 years ago, and it got approved this summer. It was developed by Loxo and is now owned by [Eli Lilly and Company]. Pralsetinib [Gavreto] is another RET-specific inhibitor. Those are the 2 newest drugs. Pralsetinib was designed by Blueprint Medicines, another excellent option. We’re going to talk about some of the data there. Cabozantinib [Cabometyx] and vandetanib [Caprelsa] are multi-TKIs. They’re not as specific as selpercatinib and pralsetinib. They do cover RET, and they are approved in RET-altered thyroid cancers, but they carry with it less efficacy and less sensitivity with more AEs than either of the 2 newer ones. Those are the 4 drugs out there that do cover RET, though the ones that we’re going to focus on are selpercatinib and pralsetinib.
Please describe the National Comprehensive Cancer Network (NCCN) guidelines for RET-targeted therapy.
If we find the RET rearrangement and it’s discovered prior to first-line therapy, the preferred option is selpercatinib or pralsetinib, and then at progression, we can go beyond that.2 It does still have category 2B consideration for cabozantinib and vandetanib, though those are older recommendations.
Now, here’s the hardest thing to discuss: a RET rearrangement discovered during first-line therapy. Do you hit pause on whatever therapy [you had prescribed]? If you chose single-agent/multiagent immunotherapy or a multiagent chemoimmunotherapy, do you stop that and shift to one of these TKIs? Because that is a consideration—interrupt therapy followed by selpercatinib. These are NCCN guidelines and something I think we need to dive into because, as with a lot of NCCN guidelines, they’re helpful, but they don’t give you the answer necessarily.
What data support the use of selpercatinib as one of these preferred treatments?
The data that got selpercatinib approved came out of the LIBRETTO-001 study [NCT03157128].3 This [included] 702 RET-altered patients. It’s the largest RET study ever. It was what started as a phase 1 study that we had at the DDU, in Nashville [for which] I gave that first dose of drug. It’s what I have 4 patients actively on therapy with. When we got into the expansion cohorts and it became the phase 2 study, it was RET fusion–positive NSCLC, RET fusion–positive nonmedullary thyroid cancer, and RET-mutated medullary thyroid cancer. These patients could be performance status 0 to 2, with good organ function and normal QT. They could have or not have brain metastases. We had 39 patients who were treatment naїve and 105 who were previously treated with chemotherapy. This is a robust study for a molecularly targeted drug with just a 2% to 3% occurrence rate in the population.
Median age was in the 60s; good balance of male and female patients in both the previously treated and untreated patients. Smoking status—most patients were not smokers, but not all of them. Most of these are adenocarcinomas. Here’s something that I found absolutely fascinating: One of the patients who was previously treated had 15 prior lines of therapy. I would like to meet both the patient and the practitioner who prescribed 15 lines of therapy in a patient with lung cancer because I would like to clone their constitution. That’s incredible. A lot of them had prior immunotherapy; 50 had prior TKI. That would be suggestive of cabozantinib or vandetanib, though I presume it could have been an EGFR inhibitor, as well. A number had brain metastases—36% in the previously treated population, 18% in the untreated population. And then the alterations...this is an important detail that I’m going to [speak to] for a second. We know in ALK that the fusion partner matters. We know in TRK that the fusion partner doesn’t matter. It seems to be based on KIF5B, CCDC6, NCOA4, and RELCH. We can see that any fusion is predictive of a response to a targeted RET inhibitor.
What were the results from the study?
Patients who had previous platinum-based chemotherapy had a 64% objective response rate [ORR] in an independent central review. Those who were untreated had an 85% ORR. If it were investigator assessed, the ORR went to 70%, and in the previously untreated population, 90%; so, an 85% ORR in untreated and a 64% ORR in previously treated. There are even a couple of complete responses [CRs], 2 of them in the previously treated group. There were, however, a couple of patients with progressive disease, as we would expect with any treatment, unfortunately.
This is an important point. The median time to response was 1.8 months, so this goes to that question of CNS disease and whether we have time to allow these drugs to work. [As with] TRK inhibitors and some of the ALK inhibitors, when a patient walks in and says, “Doc, I feel like I’m breathing better; I think this is really working,” you can believe that it’s not just wishful thinking on the part of the patient.
Even in those patients who didn’t respond, we can see pretty impressive disease control with some ongoing therapy at the time of data cutoff. This is any drug’s dream. You see that almost everybody on it is going to respond—so, a really good change in maximum tumor size on the waterfall plot for selpercatinib in the LIBRETTO-001 trial.
Among the patients who did respond—that 64% previously treated and 85% untreated—the prior therapy had a median duration of response [DOR] of 17.5 months for the median follow-up of 12 months. Now, if you go to the investigator assessment, it bumps up to 20.3 months. We have not yet reached a median DOR for those who were previously untreated, so most of those patients continued to respond after a median follow-up of 7.4 months. The response is ongoing in 63%, median follow-up of 12.1 months, so really good DOR. It’s not just a quick response and then they progress, but they can hold on to that response.
[In] 38 out of 105 patients who had prior therapy and had investigator-assessed CNS metastases at baseline, there’s an ORR of 91%. So, 10 out of 11 patients had a response, with 3 being a CR. The median DOR in the brain is 10.1 months, suggesting that we could skip the CNS toxicity that does come along with even SRS and save that for a rainy day down the road, when our patients need it; so, 91% intracranial ORR.
In further data looking at patients who had measurable disease present at the start who had had treatment or not—a bigger population; double the population, really—we looked at primary CNS overall response rate by independent review committee, and DOR was the secondary end point.4 What we saw in this larger population was an ORR of 82%—some who had had prior radiation, 75% ORR in that group—with some CRs seen, 22.7%. When you divide those up, that’s how many people had a CR to these drugs with no radiation therapy ongoing. Median DOR was out to 9.4 months [in those] who had [not had] prior radiation therapy. In the group who had prior radiation therapy, we’ve not yet reached that median DOR; again, 82% response in the brain to an oral anticancer medicine.
PFS [progression-free survival] is really important to our patients. We have a great response rate, but how long does that last? So patients who had prior chemotherapy, the independent central review showed that the median PFS was 16.5 months, 18.5 months for investigator assessment.3 The treating physician will hold on to the therapy for 2 extra months or an extra couple of cycles to prove that 12% growth was really growth or that 21% growth was really growth. We see almost a year and a half of PFS with the 1-year PFS rate of 66%. So, 2 out of 3 patients will still be on the drug without progression after being on it for a year. In the previously untreated population, that [rate] goes up to 75%; still on it at a year, with no median PFS yet determined.
Nothing that we do comes free for our patients as far as AEs, especially when we get great responses. However, with selpercatinib, and we’ll see later with pralsetinib, as well, they look good as far as tolerability. As specific as selpercatinib is, it hits VEGFR and FGFR to a much lesser degree, so I dobelieve that the hypertension is real and something that needs to be looked at closely. It caused a bit of increased AST [aspartate aminotransferase] and a bit of increased ALT [alanine aminotransferase].
With the 4 patients I have on therapy right now, the No. 1 complaint is dry mouth. You want to have a good visit with a patient: Put them on a therapy that drops their disease by 80% and ask them what their worse AE is and they say dry mouth. That makes for a great visit with that patient. Overall, symptomatically, these drugs are well tolerated; the worst symptomatic toxicity would be the grade 3 diarrhea in just 5 patients out of 144.
On May 8—this was like my second child graduating from college—selpercatinib was approved for lung and thyroid cancers with RET gene mutations or fusions.5 This was a conditional approval based upon ORR, with continued approval contingent upon later studies. In the thyroid cancer population, it is approved for adult and pediatric patients over the age of 12.
Could you discuss the impact of this approval?
There’s no question, this is not BRCA-mutated breast cancer [in terms of frequency], but [RET alterations are] out there. I think that we know that the drug companies and the sponsors for these trials always come up with an angle, and the phrase that I’ve heard for 4 or 5 different drugs in the past few months is “We’re filling an unmet need.” Who defines that, and what does that look like? For someone with a PD-L1–positive [disease], is their unmet need as much as in someone who is not? You could argue not. But, if you look at it from a targeted therapy, RET has sort of been the stepchild for the past 20 years. RET was first described in thyroid cancers in the ’80s, and there’s been no specific targeted therapy for it. I think to have a pill that someone can take and give you a year and a half as a second-line or third- line agent—or as one patient had, a 16th-line agent—[indicates some] pretty strong data.
What data support using pralsetinib in this setting?
The pralsetinib study was done by Blueprint Medicines out of Boston, [Massachusetts]. They did a phase 1/2 study called ARROW [NCT03037385]. This was a lung cancer study: overall end points, ORR and safety; secondary endpoints, DOR, clinical benefit rate—which is response plus stable disease—and disease control rate.
Looking at the [NSCLC] group, they pulled out 179 patients, so that’s a bigger lung cancer population than we saw with the LIBRETTO study; RET fusion population with intention to treat, initiated pralsetinib by July 11 of 2019. That took it down to 132, and then response-evaluable [patients] dropped that number down to 116, done by a blinded independent central review.6
So, we’re talking similar numbers when we look at these studies, though the most commonly repeated phrase at [the American Society of Clinical Oncology meeting], was “We’re not supposed to do cross-trial comparison, but we’re going to.” So, if we look at this group, broken down very similarly, median age was 60 years old, [median age in those with] prior platinum [use] was 60 [years], treatment-naїve population was a bit older [at 65 years], which I found to be interesting. Again, most of them were never smokers, but there were smokers involved in this study. The [patients with baseline] brain metastases, 40% and 41%, were so well split in this study—fairly similar numbers to what we saw in the LIBRETTO study. And then those fusion partners—again, KIF5B being the clear most favorite partner of RET, but nonmonogamously, also CCDC6 and NCOA4 were seen. We saw multiple prior therapies in this population; checkpoint inhibitors and chemotherapy, as well.
Looking at efficacy by blinded independent review, we’ll have to relate that back to the blinded portion of the LIBRETTO study. For those prior-platinum patients, the ORR was 55%; in the treatment-naїve population, it was 66% [in the] intention-to-treat [group]. In those patients who were response evaluable, the numbers went to 61% for prior platinum and 73% for treatment naïve; so, looking to be relatively comparable with what we saw with the LIBRETTO study. But there were a few more CRs that we see with pralsetinib. Disease control rates look a lot better when you start to take into account stable disease, as well. Response-evaluable [patients had] a 95% disease control rate in prior platinum patients, 88% in the treatment-naïve population; when we break it down to the clinical benefit rate, 71% in prior platinum and 73% in the treatment-naïve group.
The waterfall plot looked similar: everything going down except for a few; a good number of CRs. The median DOR was not yet reached, and 75% of responding patients continued treatment at the data cutoff; as we saw with selpercatinib, a good DOR in addition to a nice ORR.
CNS activity [was] one of the secondary outcomes for the ARROW study. There were just 9 patients [with CNS metastases at baseline in this study], but 9 versus 11 is pretty similar. We saw an intracranial ORR of 56% with a CR rate of 3%. If I’m selling selpercatinib, I’m going to say we had a 91% ORR and they had only a 56% ORR. But those are very small sample sizes, and a couple of those patients are still ongoing at this data cutoff. I think these both look to be active in the brain, and I think that over time, we’ll start to learn if one is better in the brain than the other.
How does the safety profile for pralsetinib compare with that of selpercatinib?
Remember, we saw that selpercatinib was well tolerated. We saw some hypertension, AST and ALT abnormalities, and a few other lab abnormalities. But, as far as what patients come in and tell you, they did well. We see the same thing with this. I always struggle with fatigue as a grade 3 or 4 toxicity [2.3%].7 That’s my personal bias. There was about 3% diarrhea, which matches what we saw with the selpercatinib. There was more hypertension [grade 3/4, 14%]. That is a difference we saw here [compared with what] we saw with selpercatinib. Cough [grade 3/4, 0.5%] on a lung cancer study is always a questionable thing for me.
Regarding laboratory abnormalities, some neutropenia was seen. Ten percent had grade 3/4 neutropenia; 20% had a lymphopenia, and [there was] a little bit of LFT [liver function test] abnormality, as well, but nothing dramatic jumping out that says there’s clearly end organ damage with pralsetinib.
Based on those data, 5 months later, on September 4, the FDA granted accelerated approval to pralsetinib for adult patients with metastatic RET fusion–positive NSCLC.8 There is 1 difference that I will point out: The FDA approved it in conjunction with the Oncomine Dx Target Test as the companion diagnostic. Selpercatinib, as of today, does not have a companion diagnostic approved, so you don’t have to test with a particular study. I don’t know how strict insurance would be, but there is an FDA-approved companion diagnostic for pralsetinib.
How else would you compare these 2 selective RET inhibitors?
Selpercatinib comes in 40- and 80-mg capsules. If you weigh more than or equal to 50 kg, it’s 160 mg orally twice daily. If you’re less than that, it’s 120 mg; so, a smaller dose compared with pralsetinib, which is 400 mg a day. You have to space that out around food, [which is] not necessarily true for the selpercatinib, but it is twice-a-day dosing. There are pros and cons to both.
The warnings and precautions: Selpercatinib has a lot of CYP4A interactions, so you have to watch out for that. There were some QTc prolongations, and there were some hypersensitivity reactions, usually well managed with steroids, that could be treated through. Pralsetinib, though, had some pneumonitis that was seen with it, as well. You look at all those toxicities, you look at the dosing, and you see a treatment- naїve ORR of 85% versus 66%, a previously treated ORR of 64% versus 55%, and intracranial ORRs of 91% versus 56%—again, small numbers. Data are evolving, but these are the numbers we have right now; so, 2 great options for our patients with RET-fused lung cancer.
REFERENCES
1. Kato S, Subbiah V, Marchlik E, Elkin SK, Carter JL, Kurzrock R. RET aberrations in diverse cancers: next-generation sequencing of 4871 patients. Clin Cancer Res. 2017;23(8):1988-1997. doi:10.1158/1078-0432.CCR-16-1679]
2. NCCN Clinical Practice Guidelines in Oncology. Non-small cell lung cancer, version 2.2021. December 15, 2020. Accessed January 5, 2021. https://bit.ly/35kO18V
3. Drilon A, Oxnard GR, Tan DSW, et al. Efficacy of selpercatinib in RET fusion–positive non– small-cell lung cancer. N Engl J Med. 2020;383:813-824. doi:10.1056/NEJMoa2005653
4. Subbiah V, Gainor JF, Oxnard GR, et al. Intracranial activity of selpercatinib (LOXO-292) in RET fusion-positive non-small cell lung cancer (NSCLC) patients on the LIBRETTO-001 trial. J Clin Oncol. 2020;38(suppl 15):9516. doi:10.1200/ JCO.2020.38.15_suppl.9516
5. FDA approves selpercatinib for lung and thyroid cancers with RET gene mutations or fusions. FDA. May 11, 2020. Accessed January 5, 2021. https://bit.ly/3hPMahq
6. Gainor JF, Curigliano G, Kim DW, et al. Registrational dataset from the phase I/II ARROW trial of pralsetinib (BLU-667) in patients (pts) with advanced RET fusion+ non- small cell lung cancer (NSCLC). J Clin Oncol. 2020;38(suppl 15):9515. doi:10.1200/ JCO.2020.38.15_suppl.9515
7. Gavreto. Prescribing information. Blueprint Medicines Corp; 2020. Accessed January 5, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213721s000lbl.pdf
8. FDA approves pralsetinib for lung cancer with RET gene fusions. FDA. September 8, 2020. Accessed January 5, 2021. https://bit.ly/3nm0C1I

Bispecific Antibodies and ADCs Deliver a Futuristic Horizon Across Lung Cancer Settings
October 23rd 2024Recent advancements in protein engineering, especially antibody-drug conjugates, show promise in lung cancer treatment, with ivonescimab outperforming pembrolizumab in PD-L1-positive advanced non-small cell lung cancer.
Read More