HT Scoring Identifies Risk and Outcomes of CAR T Therapy for MCL
The CAR-HEMATOTOX score was positively associated with identifying the risk of poor treatment outcomes for patients with mantle cell lymphoma treated with chimeric antigen receptor T-cell therapy.
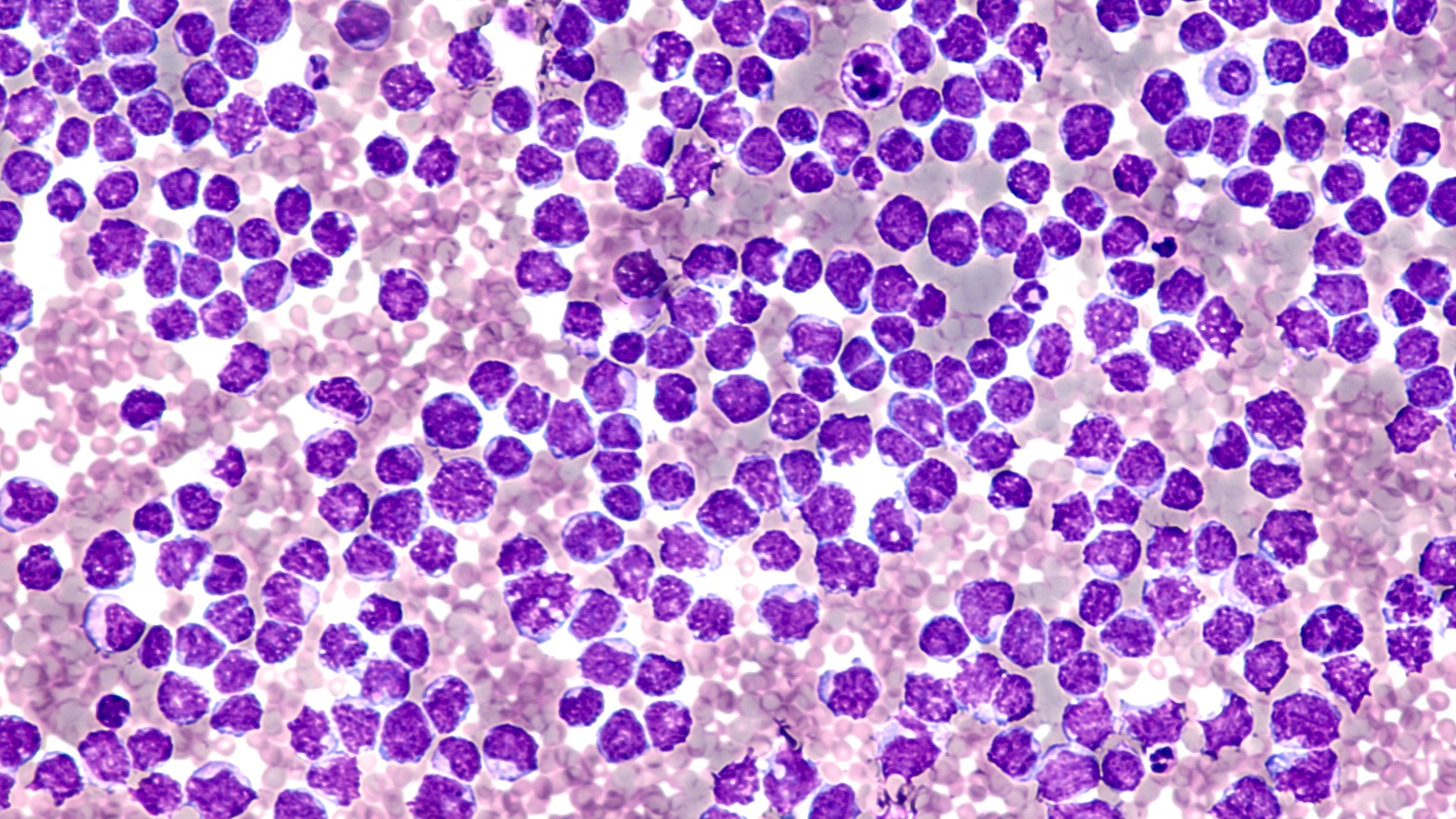
Malignant cells of mantle cell lymphoma: © David A Litman - stock.adobe.com
Analyses show that a hematoxicity scoring system could identify poor treatment outcomes for patients with mantle cell lymphoma (MCL) treated with brexucabtagene autoleucel (brexu-cel; Tecartus) chimeric antigen receptor (CAR) T-cell therapy, according to a study in the American Journal of Hematology.1
A high CAR-FYI HEMATOTOX (HT) score was independently associated with severe hematoxicity, higher incidence of infection, and poor progression-free survival (PFS) and overall survival (OS) rates.
In the study, the cohort with high HT scores experienced prolonged neutropenia (median 14 v 6 days; P < .001) and an increased rate of infection (30% v 5%; P = .001). Patients with high HT scores also experienced worse 90-day complete response rates (68% v 93%; P = .002), PFS (median 9 months v not-reached; P < 0.0001), and OS (median 26 months v not reached; P < .0001). Low HT scores were also associated with improved overall response (100% v 85%; P = 0.003).
According to authors of the study, “the HT score enables early risk-stratification of [patients with] MCL into high vs low risk for prolonged neutropenia, severe infections, and poor survival outcomes prior to brexu-cel infusion.” The authors added that the score could also help clinicians identify “ultra-high-risk patients in need of further treatment optimization.”1
Investigators assessed 103 patients with relapsed or refractory MCL receiving brexu-cel at a median follow-up of 15.4 months. The median age was 66 years (range, 49-89), and patients received a median of 3 prior treatment lines.1 Patient HT scores were calculated on the day of lymphodepletion (day -5) using the German Lymphoma Alliance’s calculator. The calculator accounts for 5 metrics of hematoxicity, including platelet count, absolute neutrophil count, hemoglobin, C-reactive protein, and ferritin, with additional weighting of the baseline platelet count and ferritin levels.2 Fifty-six patients had low HT scores (0-1) and 47 patients had high HT scores (2-7). The median HT score was 1.1
Patients with high HT scores more often exhibited an aplastic phenotype of neutrophil recovery, which was not observed in the low HT score group (47% vs 0%; P < .0001). Investigators observed a significant positive correlation between HT score and duration of severe neutropenia. The high HT group also had more patients with prolonged neutropenia (66% v 30%; P = .0004).
Furthermore, patients with high HT scores experienced higher rates of early (until day +30) and late (day +31 to day +100) severe thrombocytopenia and anemia. These conditions led to more required platelet transfusions.
Regarding infection rates, the high HT group experienced more infections of any grade (43% v 25%; P = .09) and more severe infections (30% v 5%; P = .01). No fatal infection was observed in the low HT group, while 7 deaths were attributed to infection in the high HT group.
Study authors noted some limitations, which include that their analysis was retrospective and uncontrolled, and follow-up still remains short. Further analysis should evaluate HT score in a prospective manner, and response assessment should be performed by an independent review committee, according to authors.1
REFERENCES
1. Rejeski K, Wang Y, Albanyan O, et al. The CAR-HEMATOTOX score identifies patients at high risk for hematological toxicity, infectious complications, and poor treatment outcomes following brexucabtagene autoleucel for relapsed or refractory MCL [published online ahead of print, 2023 Aug 16]. Am J Hematol. 2023;10.1002/ajh.27056. doi:10.1002/ajh.27056
2. Scores. German Lymphoma Alliance. Accessed October 9, 2023. https://tinyurl.com/2uy7cath
Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen