Positive Outcomes With Immunochemotherapy and Lenalidomide TP53WT MCL
Findings from a phase 2 study show that sequential minimal residual disease assessment is a powerful prognostic tool in patients with mantle cell lymphoma.
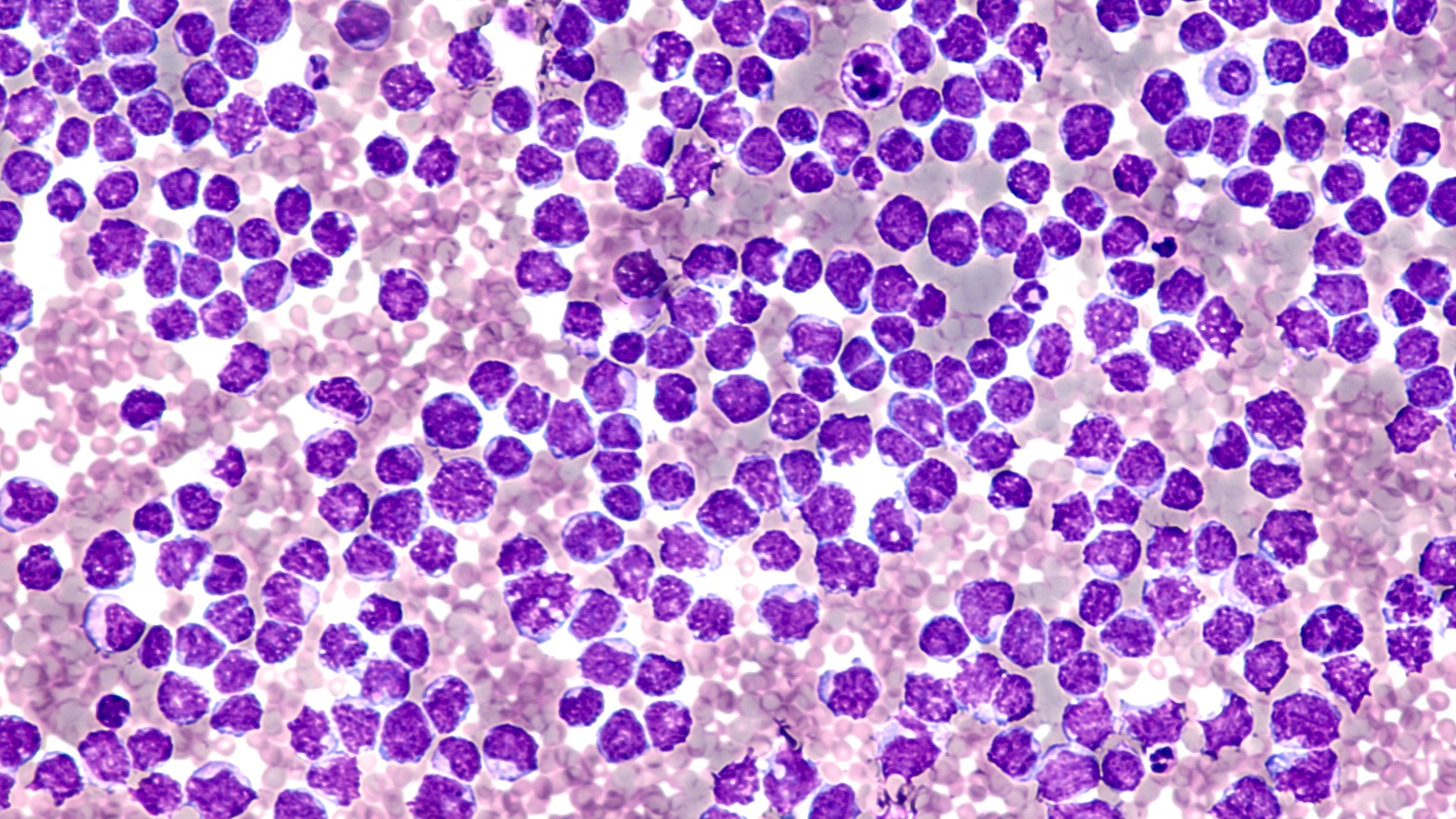
malignant cells of a mantle cell lymphoma: © David A Litman - stock.adobe.com
While the primary end point of 3-year progression-free survival (PFS) was not met, favorable outcomes were observed with immunochemotherapy with lenalidomide (Revlimid), without autologous stem cell transplant consolidation among patients with TP53-wild-type mantle cell lymphoma (MCL), including patients who are at high-risk, according to data from a phase 2 study (NCT02633137) published in Haematologica.1
The median follow-up among survivors was 63 months (range, 11-, 84). By intent-to-treat, the overall response rate was 88% (n = 43) and were all complete responses, including 1 patient who had stable disease, and 2 patients who had disease progression during the study.
The 3-year PFS rate was 63% (95% CI, 50-78), not meeting the study's primary end point, and differed by TP53 status with 78% wild-type vs 38% ALT (P =.043). The median overall survival (OS) at 3 years was 85% (95% CI, 76-96).
“Although the primary study end point of 3-year PFS was not met, this was primarily driven by the poor outcomes observed among patients with TP53-aberrant MCL, further establishing that TP53-aberrant MCL is associated with poor outcomes when treated with [immunochemotherapy] and lenalidomide does not overcome this negative prognostic impact,” wrote study authors in findings published in Haematologica.
In the single-center, investigator-initiated, phase 2 study, patients aged ≥ 18 years with untreated stage II-IV MCL were enrolled if they had radiographically measurable disease, absent active infection, absent central nervous system involvement by MCL, and adequate performance status, blood counts, and organ function.2
A total of 49 patients were enrolled from January 2016 to June 2018, and those who were efficacy-evaluable completed lenalidomide combined with rituximab (Rituxan) plus cyclophosphamide, doxorubicin, vincristine, and prednisone (len-R-CHOP) treatment. Two patients did not complete len-R-CHOP: , 1 for progressive disease, and 1 for toxicity. One patient withdrew from the study in remission following rituximab and cytarabine (R-HiDAC) to pursue high-dose therapy with autologous stem cell rescue.1
Among those enrolled, the median age was 63 years (range, 30-79), 22 (45%) patients were ≥65 years old at enrollment, and 31 (65%) patients were high-risk by protocol. This included 4 patients with blastoid histology. For mutations, 41 (84%) patients had tumor TP53 mutation and deletion status, 14 of which were TP53 aberrant (34%). Three of these patients harbored mutated TP53, 5 harbored one copy of TP53, and 6 patients harbored both. Forty-seven patients ended up being response evaluable.
The primary end point was the rate of PFS at 3 years. Minimal residual disease (MRD) was measured using a next-generation sequencing (NGS)-based assay after each phase of treatment and at 6 months following end-of-treatment.
Additional findings showed that all but 3 response-evaluable patients with localized relapsed MCL amenable to radiation were given BTKi-based therapy. Eight received single-agent and 18 combination therapy, and 19 (76% of response-assessed) patients had disease response.
Nine patients had TP53 mutation at relapse and received BTKi. Of these patients, 7 (78%) experienced disease response. For patients who were relapsing/progressing, the median OS was 32 months (95% CI, 19-not reached [NR]) from time of relapse/progression. Further, the 7 patients who progressed within 2 years of diagnosis had a median OS of 17 months (95% CI, 7-NR) after the 2-year time point vs a median that was not reached for the 38 non-progressing patients (P <.001).
For safety, no treatment-related deaths were observed in the study. The most common grade ≥3 toxicities were hematologic with the most frequent being neutropenia, which occurred in 37% of patients undergoing len-R-CHOP, 70% of patients undergoing R-HiDAC, and 42% of patients receiving R-len. Rates of febrile neutropenia occurred in 14%, 21%, and 7%, and grade ≥3 thrombocytopenia was seen in 22%, 83%, and 9% in the 3 treatment phases, respectively.
Treatment-related adverse events led to dose reductions or delays in 41% of patients receiving len-R-CHOP, 36% treated with R-HiDAC, and 53% given R-len. Twenty patients required dose reduction/delay during len-R-CHOP due to neutropenic fever (n = 7), cytopenia (n = 7), infection (n = 3), rash (n = 2), or other causes (n = 2).
Moreover, rare grade ≥3 infections occurred, including pneumonia (n = 4), skin/soft tissue (n = 1), and sepsis (n = 1), and frequent grade ≤2 toxicities across phases of treatment included fatigue (35% during len-R-CHOP), peripheral sensory neuropathy (29% during len-R-CHOP), and rash (20% during both len-R-CHOP and R-len).
Of the 37 patients with MRD results at the level of 1 x 10-5 sensitivity at end of treatment, 4 were detectable MRD (dMRD), 2 of which were simultaneous with relapse. All 6 patients whose MCL was uMRD at the level of 1 x 10-6 sensitivity at end of treatment converted to dMRD at 6 months post-end of treatment eventually experienced disease relapse. For the 29 patients with level of 1 x 10-6 sensitivity results, including 12 dMRD and 17 undetectable MRD, median PFS was 42 months (95% CI, 34-NR) for uMRD vs 11 months (95% CI, 0-NR) for dMRD (P < .001).
In a high-dose, therapy-sparing, intensive approach, favorable outcomes were seen in patients with TP53-wild-type MCL, including high-risk cases. These data demonstrate that sequential MRD assessment is a powerful prognostic tool in patients with MCL.
“Overall, we have shown that MRD status carried prognostic importance in our sequential treatment regimen, especially at later time points such as 6 months following end of treatment, and that 1 x 10-6 is more strongly predictive of outcomes than 1 x 10-5 sensitivity,” concluded the study authors.
REFERENCES:
Epstein-Peterson ZD, Drill E, Aypar U, et al. Immunochemotherapy plus lenalidomide for high-risk mantle cell lymphoma with measurable residual disease evaluation [published online ahead of print, 2023 Aug 31]. Haematologica. 2023;10.3324/haematol.2023.282898. doi:10.3324/haematol.2023.282898
Sequential chemotherapy and lenalidomide followed by rituximab and lenalidomide maintenance for untreated mantle cell lymphoma. ClinicalTrials.gov. Updated February 21, 2023. Accessed October 13, 2023. https://tinyurl.com/39k5pde4
Liso-Cel Delivers Deep, Durable Responses in R/R MCL
January 11th 2024High complete response rates and low incidences of cytokine release syndrome and neurological events were observed when patients with relapsed or refractory mantle cell lymphoma were treated with lisocabtagene maraleucel.
Read More
ZUMA-18 Study Shows Brexu-cel's Therapeutic Potential in MCL
January 3rd 2024In an interview with Targeted Oncology, Andre Goy, MD, discussed the potential of brexucabtagene autoleucel for the treatment of patients with relapsed/refractory mantle cell lymphoma and how 2 studies provide support for use of the agent in this patient population.
Read More