Updated BRUIN Data Shows High Response Rates With Pirtobrutinib in CLL/SLL
In an interview with Targeted Oncology, Jennifer A. Woyach, MD, discussed updated results from the phase 1/2 BRUIN study of pirtobrutinib in chronic lymphocytic leukemia or small lymphocytic lymphoma following treatment with a covalent Bruton tyrosine kinase inhibitor.
Jennifer A. Woyach, MD

After treatment with a covalent Bruton tyrosine kinase (BTK) inhibitor, heavily pretreated patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) showed high objective response rates (ORR) and progression-free survival (PFS) outcomes when treated with pirtobrutinib (Jaypirca), according to updated results from the phase 1/2 BRUIN study (NCT03740529).1
At the American Society of Hematology 2023 Annual Meeting, Jennifer A. Woyach, MD, discussed new results from the BRUIN study which come from a median follow-up of 30 months. At this time, treatment with pirtobrutinib led to an ORR of 81.6% (95% CI, 76.5%-85.9%) in the 282 patients included in the population. This included a complete response (CR) rate of 1.8%, a partial response (PR) rate of 69.5%, a nodular PR (nPR) of 0.7%, and PR with lymphocytosis (PR-L) of 9.6%.
Regardless of prior BCL-2 exposure, pirtobrutinib generated an ORR of approximately 80%. Among the 154 patients who were naive to BCL-2 inhibition, the ORR was 83.1% (95% CI, 76.2%-88.7%) with pirtobrutinib, including a CR rate of 3.2%, a nPR rate of 1.3%, a PR of 70.1%, and a PR-L rate of 8.4%. For the 128 patients who had prior exposure to BCL-2 inhibitors, the ORR was 79.7% (95% CI, 71.7%-86.3%), and included a PR rate of 68.8% and a PR-L rate of 10.9%.
At a median follow-up of 27.5 months, patients previously treated with covalent BTK inhibitors had a median PFS of 19.4 months (95% CI, 16.6-22.1) with pirtobrutinib, and at a median follow-up of 27.6 months for patients in the BCL-2 inhibitor-naive group, the median PFS was 23.0 months (95% CI, 19.6-28.4). Further, with a median follow-up of 22.2 months, patients included in the BCL-2 inhibitor-exposed group had a median PFS of 15.9 months (95% CI, 13.6-17.5).
For overall survival (OS), patients in the the total population of patients who previously received a covalent BTK inhibitor had a median OS that was not evaluable (NE; 95% CI, NE-NE) at a median follow-up of 29.3 months. Among those who were naive or exposed to BCL-2 inhibitors, the median OS at a median follow-up of 31.6 months and 27.4 months was NE (95% CI, NE-NE) and NE (95% CI, 28.4-NE), respectively.
In an interview with Targeted OncologyTM, Woyach, a hematologist-oncologist, professor in the Division of Hematology at The Ohio State University, and co-leader of the Leukemia Research Program at The Ohio State University Comprehensive Cancer Center, discussed these updated results from the phase 1/2 BRUIN study.
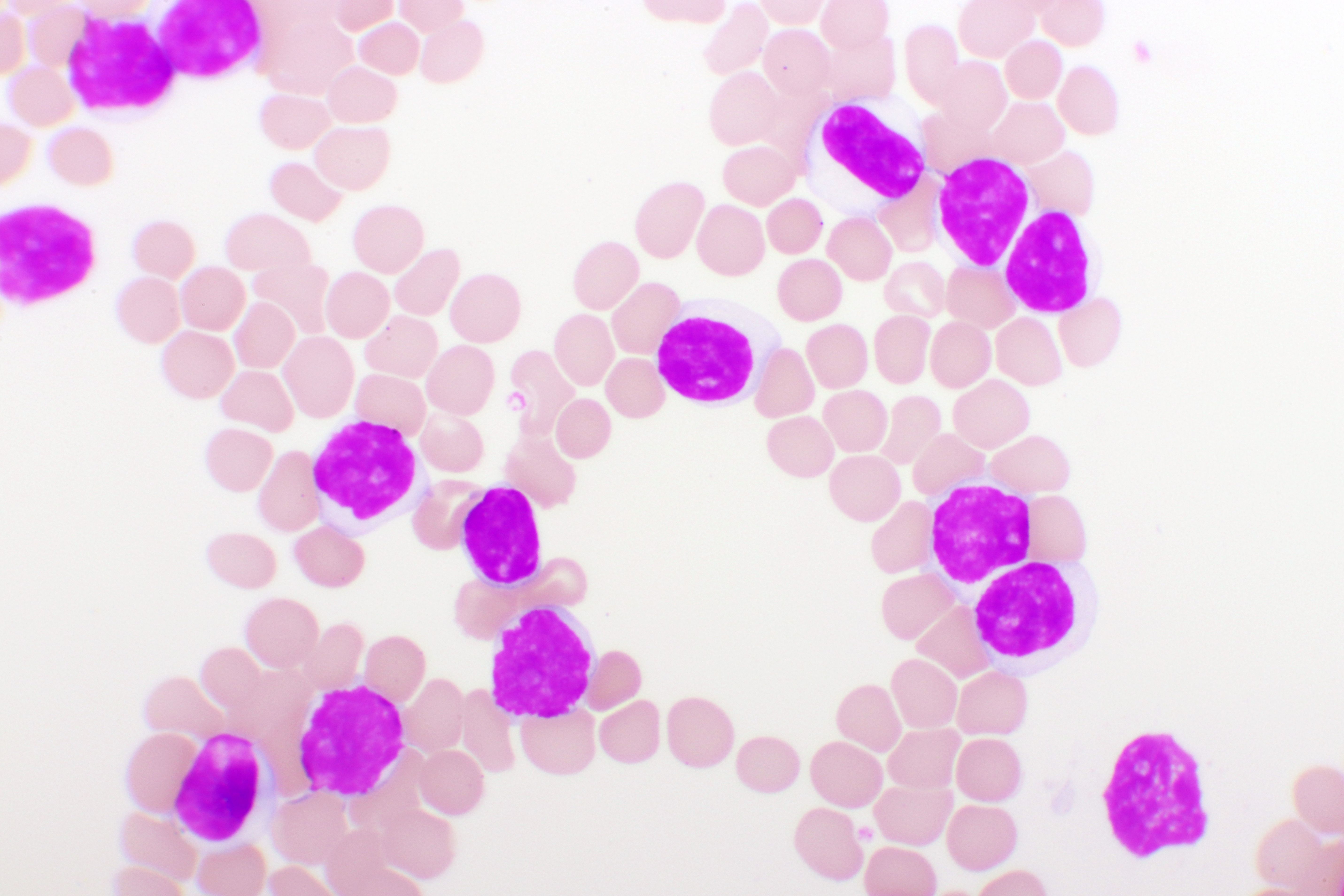
Blood smear of chronic lymphocytic leukemia (CLL), analyze by microscope: © jarun011 - stock.adobe.com
Targeted Oncology: Can you provide an overview of the 30 months follow-up and subgroup analysis of the phase 1/2 BRUIN study?
Woyach: We discussed the long-term follow-up of pirtobrutinib in patients with relapsed/refractory CLL, which is a follow-up of the BRUIN phase 1/2 trial. Here, we had about 30 months of follow-up on the study, and focused specifically on the group of patients who had received a prior covalent BTK inhibitor, so either ibrutinib [Imbruvica], acalabrutinib [Calquence], zanubrutinib [Brukinsa]. This cohort was about 280 patients. Then, we broke that cohort down further into the patients who had previously been treated with the BCL-2 inhibitor and the patients who were previously naive to a BCL-2 inhibitor.
What were the main findings highlighted at the meeting?
Overall response rate has been reported before [and] it's over 80%. It did not vary based upon whether patients had received a prior BCL-2 inhibitor or not. We also see with long-term follow-up [that the] median progression-free survival is 19.4 months for that entire cohort. This did look a little bit different in the patients who had previously been treated with a BCL-2 inhibitor and those that had not.
Those patients who had received a prior BCL-2 inhibitor had a median progression-free survival of about 16 months. Those that had not had a median PFS of about 23 months. Importantly, the patients who had received a prior BCL-2 inhibitor, as you would expect, were just a higher-risk group of patients in general. They obviously had had more prior therapies, a number of them had either [chimeric antigen receptor] T cells or even allogeneic stem cell transplants, showing us that the later in lines of therapy, the PFS is going to be shorter.
What else can you highlight regarding response rate?
We looked further at response rate in some different patients subgroups between the BCL-2 naive and the BCL-2 exposed subgroup. There weren't a lot of surprising trends there. There was a trend toward a lower response rate in patients with [phospholipase C gamma 2] mutations. That's the protein immediately downstream of BTK. [One] would expect that a mutation there might lead to a lower response rate. Importantly, higher risk characteristics, so things like TP53 alterations and IGHV unmutated disease didn't seem to affect response rate.
For safety, what were the most common adverse effects observed?
Pirtobrutinib has been exceptionally well tolerated in clinical trials. Most of the toxicities are grades 1 and 2. The more common things we see are some common toxicities. In general, people tend to sometimes have some gastrointestinal [adverse] effects. Bruising is common [and] neutropenia was fairly common among the cytopenia toxicities. When looking at adverse [effects] of special interest, things that we think about with BTK inhibitors, like atrial fibrillation, hypertension, bleeding rates, all were very low. There was about a 4% rate of atrial fibrillation, but a 4% risk of higher-grade hypertension, and high-grade bleeding was about 2%.
Overall, how does this agent compare with other BTK inhibitors?
Pirtobrutinib should be thought of as distinct from the other commercially available BTK inhibitors because this is a non-covalent inhibitor, as opposed to the other ones, which are covalent inhibitors. An [adverse] effect profile might be a little bit better with pirtobrutinib because it is such a selective molecule. So far, it's only been tested in the post-covalent BTK inhibitor setting in large numbers of patients. This is the subset of patients where accelerated approval was achieved recently, so that's for patients with relapsed/refractory CLL, who have received both a prior BTK and a prior BCL-2 inhibitor.
What are the next steps moving forward?
As mentioned, pirtobrutinib just got accelerated approval in CLL. There are a number of phase 3 trials that are ongoing, either accruing patients or where we are just awaiting results. This is looking at pirtobrutinib in a number of different clinical settings from the relapsed/refractory setting all the way up through frontline disease.
REFERENCE:
Woyach JA, Brown JR, Ghia P, et al. Pirtobrutinib in post-cBTKi CLL/SLL: ~30 months follow-up and subgroup analysis with/without prior BCL2i from the phase 1/2 BRUIN study. Ann Oncol. 2023;142(suppl 1):325. doi:10.1182/blood-2023-185852
Considering the Durability of Zanubrutinib in Relapsed/Refractory CLL
April 11th 2024During a Case-Based Roundtable® event, Marc S. Hoffmann, MD, discussed his viewpoints on the use of Bruton tyrosine kinase inhibitors for patients with relapsed/refractory chronic lymphocytic leukemia and the efficacy behind zanubrutinib in the second article of a 2-part series.
Read More