Burns Compares Therapies Approved for NSCLC With an EGFR Exon 20 Insertion Mutation
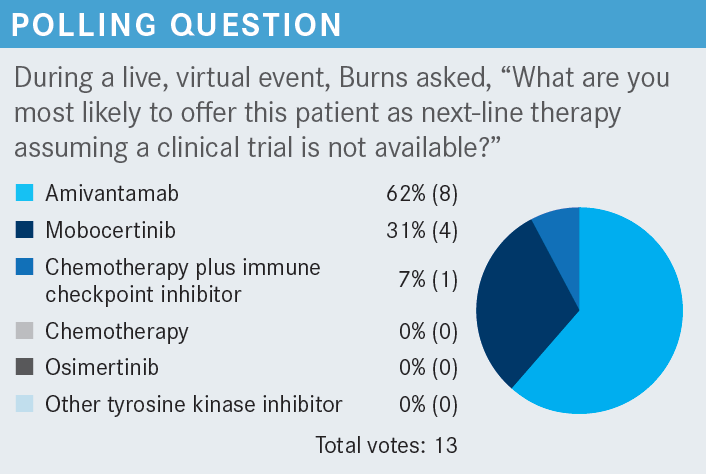
During a Targeted Oncology™ Case-Based Roundtable™ event, Timothy F. Burns, MD, PhD, discussed the trials supporting the use of mobocertinib and amivantamab for patients with non–small cell lung cancer and an EGFR exon 20 insertion.
Timothy F. Burns, MD, PhD
Associate Professor of Medicine
Associate Program Director for Research, Hematology/Oncology Fellowship Program
Department of Medicine
Division of Hematology-Oncology
UPMC Hillman Cancer Center
Pittsburgh, PA

CASE
- A 56-year-old woman presented with persistent cough and mild progressive dyspnea over the past month, with some chest discomfort, especially during routine exercise.
- She is a mother of 2 teenage children, a former light smoker, with no other notable medical history.
- ECOG performance status: 1
- CT/PET-CT shows mass in right lower lobe, right pleural metastasis, and right malignant pleural effusion.
- Brain MRI is negative for brain metastases.
- Transbronchial lung biopsy shows adenocarcinoma.
- Tissue next-generation sequencing showed EGFR exon 20 insertion mutation (V769_D770insASV).
- PD-L1 expression negative
- The patient received carboplatin/pemetrexed chemotherapy and achieved a partial response.
- Four months later, the patient reported worsening back pain and shortness of breath.
- CT scan shows progression in primary tumor and a new adrenal metastasis.
- Repeat brain MRI shows no metastases.
Targeted OncologyTM: What drugs have been approved for second-line use in patients with non– small cell lung cancer (NSCLC) and an EGFR exon 20 insertion mutation?
BURNS: There are 2 drugs that are currently approved in the second-line setting. We have mobocertinib [Exkivity], which is a tyrosine kinase inhibitor [TKI] that is similar in structure to the other TKIs but has a shorter foot that fits into the kinase domain. It seems to work where some of the others don’t. So that’s the traditional TKI.1
The other drug, amivantamab-vmjw [Rybrevant], is quite unique. It’s a bispecific antibody. One arm targets EGFR; the other arm targets MET. There are several reasons why this might be a good idea. One, MET seems to be a common mechanism of resistance. In addition, the EGFR-MET pathway has been [shown to have crosstalk], so this [drug] allows you to bind both, causing the receptors to be internalized, and if the receptor is not in the membrane, it can’t signal. In addition, there may be some immune effects, mostly by natural killer cells and macrophages.1 It’s nice that we have 2 very distinct, potentially nonoverlapping therapies.
Which trial investigated the use of mobocertinib in this setting?
Mobocertinib was initially approved [based on the data from the] EXCLAIM trial [NCT02716116]. There was initially dose escalation to find a safe dose and then it was expanded in a number of cohorts. I am focusing on the data [that supported] its approval in patients with EGFR exon 20 insertion–positive NSCLC, previously treated [with platinum therapy].2
The patient characteristics were what you might expect, with a female predominance [66%] and more patients who were Asian [60%] than Black or White. Almost all had adenocarcinoma [98%] and most were never smokers [71%], but approximately one-third were former smokers. I want to point out that these were heavily pretreated patients; the vast majority had 2, 3, or more prior lines of therapy. All of the patients had a platinum doublet [and 43%] had immunotherapy [IO]. If you break that down, it was somewhat equally divided between IO monotherapy vs chemotherapy plus IO. Some patients had received EGFR TKIs [25%] and there were patients with brain metastases in this study.2
What was the efficacy in the EXCLAIM trial?
The objective response rate was 28% [95% CI, 20%-37%] by central review and 35% by investigator. So this was a decent response rate, greater than we had seen in the past. Most impressive was the duration of response [DOR], which was 17.5 months. The respondents seemed to have durable responses and the median overall survival [OS] was 24 months.
We had an update of these data at the European Society for Medical Oncology Congress in 2022 [and the results were consistent with the earlier data]. Most patients had partial responses and again, the durability seemed to be the most remarkable thing.3
Among patients who had received EGFR TKIs, [including] investigational drugs poziotinib and osimertinib [Tagrisso], all had at least some response.4
This drug is like a typical EGFR TKI so, not unexpectedly, the dominant adverse event [AE] was diarrhea. Diarrhea of any grade affected 91% of patients and diarrhea of grade 3 affected 21%. Rash, paronychia, dry skin, and nausea also occurred, but the most common AE was the diarrhea. As with all TKIs, there was a risk of pneumonitis, cardiomyopathy, and QT prolongation.2,5
What data support the use of the other approved second-line drug, amivantamab, the bispecific antibody?
[Those data came from] the CHRYSALIS study [NCT02609776], which also had multiple arms and had a dose escalation [followed by] expansion. These patients had to have had prior lines of therapy and a good performance status, and previously treated brain metastases were allowed, similar to the EXCLAIM trial of mobocertinib. We’re going to focus on cohort D, which produced exciting data looking in patients with EGFR exon [20 insertions].6
[The baseline characteristics of this study’s patient population were] somewhat similar to those of the EXCLAIM trial of mobocertinib. There were more female than male patients [approximately 60% female], more Asian than White or Black patients [approximately 50% to 60% Asian], and most were never smokers, though in the efficacy population, almost half [were smokers].
The median time from initial diagnosis was 17 months in [the efficacy population] and most patients had adenocarcinoma [95%], though some had squamous cell carcinoma. The median number of prior lines of therapy [in the efficacy population] was 2. Forty-six percent of patients had received an IO, all had received chemotherapy, and 25% had received an EGFR TKI.
How did patients on the CHRYSALIS trial respond to treatment?
There was an impressive overall response rate of 40% [95% CI, 29%-51%] according to central review, which was higher than [the investigator-reported value of 36%. With respect to the location of the exon 20 insertions,] there were responses [when the insertion was located] across the helical region, the narrow loop, and the far loop. The median DOR was 11.1 months and median PFS was 8.3 months. The immature median OS was 22.8 months, comparable to [that reported in the EXCLAIM trial].6
Again, these are drugs that target EGFR so, as was seen with mobocertinib, rash is observed with these drugs and paronychia is very common. Unique to amivantamab is the infusion reaction [that is reported to occur] in two-thirds of patients.6 I had 6 or 7 patients on amivantamab and each has had an infusion reaction. So I tell my patients: “This is a good drug, but [during] that first cycle, you’re going to have an infusion reaction. When you do, this is what we’re going to do to treat it.”
It’s not life-threatening but it can be very scary, so I think it’s unfair to a patient to not prepare them for that infusion reaction because they will have something. Most of these AEs are relatively mild but they are disturbing to the patient, so I think giving a heads up to the patient, setting their expectation, is helpful because this is only with the first dose.
Most of the grade 3 AEs were infusion reactions. There was a discontinuation rate of approximately 7%, a dose reduction rate of approximately 10%, and a dose interruption rate of approximately 34%.
How do mobocertinib and amivantamab compare with respect to practical considerations?
Amivantamab is an intravenous infusion; mobocertinib is a pill. This is key for that first week. Amivantamab is given weekly for the first 4 weeks, but the first dose is split into 2 [doses, on day 1 and day 2], and that’s because of the infusion reaction. It’s very important to premedicate these patients aggressively prior to day 1.
There are many overlapping AEs, and there are some unique ones, such as the infusion reaction you see with amivantamab. You do see edema [with amivantamab]. Both drugs can cause low levels of interstitial lung disease and pneumonitis. There are also some reports of ocular toxicity [with amivantamab].5,7
REFERENCES
1. Friedlaender A, Subbiah V, Russo A, et al. EGFR and HER2 exon 20 insertions in solid tumours: from biology to treatment. Nat Rev Clin Oncol. 2022;19(1):51-69. doi:10.1038/s41571-021-00558-1
2. Zhou C, Ramalingam SS, Kim TM, et al. Treatment outcomes and safety of mobocertinib in platinum-pretreated patients with EGFR exon 20 insertion-positive metastatic non-small cell lung cancer: a phase 1/2 open-label nonrandomized clinical trial. JAMA Oncol. 2021;7(12):e214761. doi:10.1001/jamaoncol.2021.4761
3. Ramalingam, S. Phase I/II study of mobocertinib in EGFR exon 20 insertion (ex20ins) + metastatic NSCLC (mNSCLC): updated results from platinum-pretreated patients. Ann Oncol. 2022;33(suppl 7):S448-S554. doi:10.1016/annonc/annonc1064
4. Spira A, Ramalingam S, Neal J, et al. Mobocertinib in EGFR exon 20 insertion–positive metastatic NSCLC patients with disease control on prior EGFR TKI therapy. Presented at: International Association for the Study of Lung Cancer 2021 World Conference on Lung Cancer; September 8-14, 2021; Virtual. Abstract OA15.01.
5. Exkivity. Prescribing information. Takeda Pharmaceuticals America; 2021. Accessed February 3, 2023. https://bit.ly/3I3DqSn
6. Park K, Haura EB, Leighl NB, et al. Amivantamab in EGFR exon 20 insertion-mutated non-small-cell lung cancer progressing on platinum chemotherapy: initial results from the CHRYSALIS phase I study. J Clin Oncol. 2021;39(30):3391-3402. doi:10.1200/JCO.21.00662
7. Rybrevant. Prescribing information. Janssen Biotech; 2022. Accessed February 2023. https://bit.ly/3HLX70u
Brown Examines Lenvatinib/Pembrolizumab Combination in pMMR Endometrial Cancer
May 17th 2024During a Case-Based Roundtable® event, Jubilee Brown, MD, discussed the efficacy and safety data from the KEYNOTE-775/Study 309 trial of lenvatinib plus pembrolizumab in patients with mismatch repair proficient advanced endometrial cancer.
Read More
How Data Help Physicians Improve Operations and Achieve Health Equity
May 13th 2024A US health care executive survey found 30% see health equity solely as a social concern. Yet, it's about ensuring everyone has a fair shot at optimal health. Utilizing standardized data can shift care from reactive to preventive, easing strain on systems.
Read More