L-MIND Trial Results Show CD19 Antibody Is Reasonable in R/R DLBCL
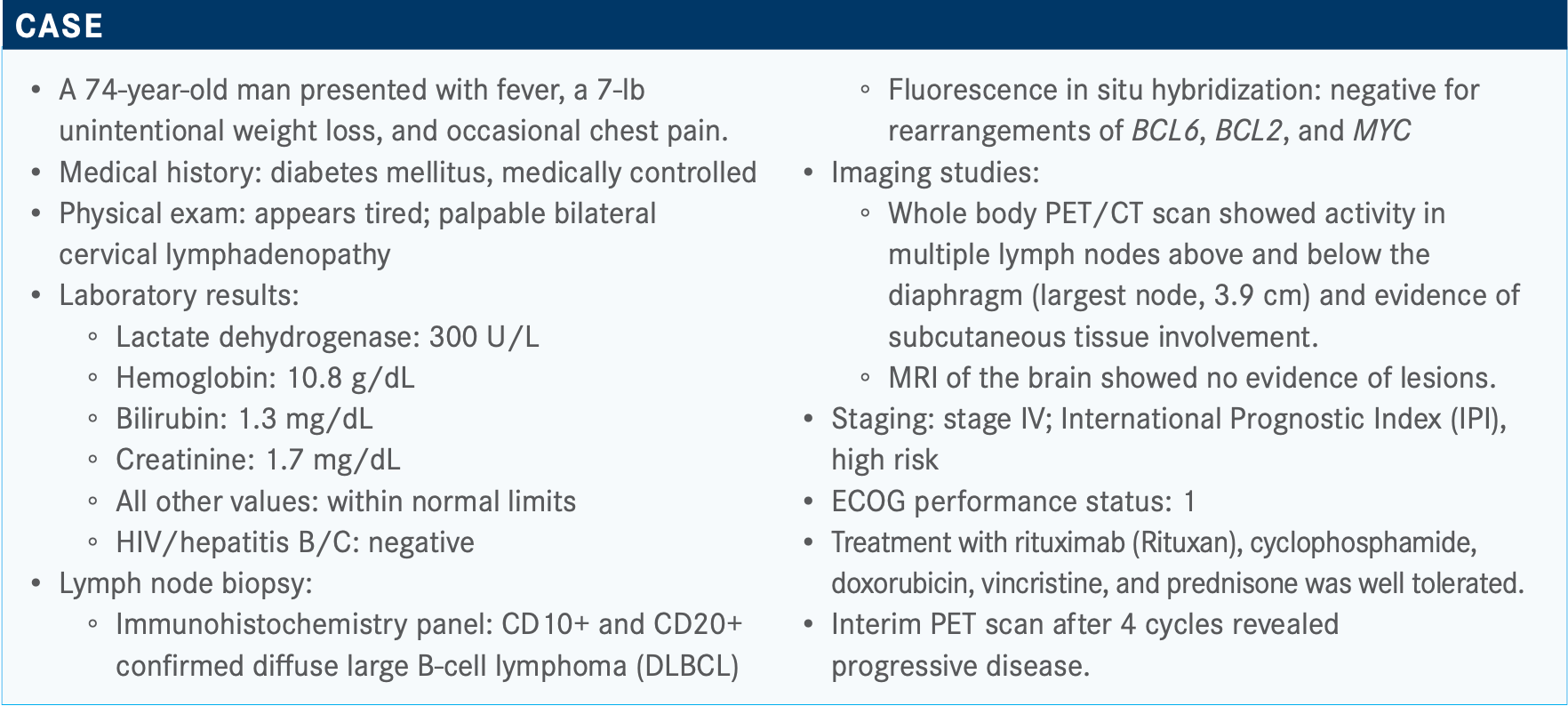
During a Targeted Oncology Case Based Peer Perspectives Roundtable event, Loretta J. Nastoupil, MD, discussed the case of a 74-year-old patients with diffuse large B-cell lymphoma.
Loretta J. Nastoupil, MD

During a Targeted Oncology Case Based Peer Perspectives Roundtable event, Loretta J. Nastoupil, MD, associate professor, director, Lymphoma Outcomes Database, section chief, New Drug Development, in the Department of Lymphoma/Myeloma, Division Cancer Medicine, at The University of Texas MD Anderson Cancer Center, discussed the case of a 74-year-old patients with diffuse large B-cell lymphoma.
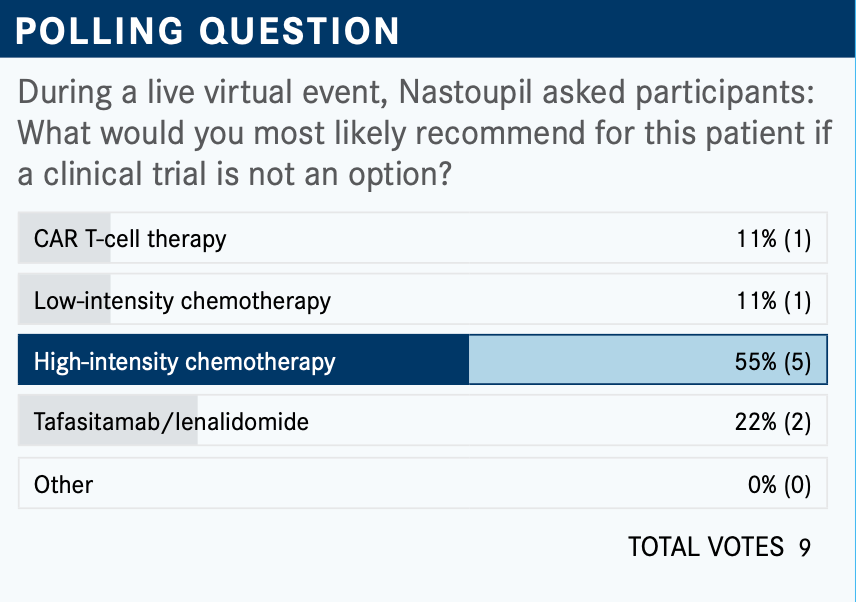
Targeted OncologyTM: What are the potential second- and third-line therapy options for this patient at this point in their treatment?
NASTOUPIL: The current NCCN [National Comprehensive Cancer Network] guidelines...look like a laundry list of a number of different therapeutic options and [do] not necessarily provide an algorithm for what might be the preferred choice based [on] certain patient characteristics.1 It just signifies that there may be several different chemoimmuno-therapy approaches and then even some potential targeted therapy approaches.
Then in the third line, CAR [chimeric antigen receptor] T-cell therapy becomes an option for patients.
Why is the tafasitamab and lenalidomide regimen listed in this poll? What is the rationale for combining these agents?
For those who may not be familiar, tafasitamab is a naked CD19 antibody, not a CAR T therapy. It’s not an antibody-drug conjugate but a naked antibody engineered for enhanced ADCC [anti- body-dependent cellular cytotoxicity].
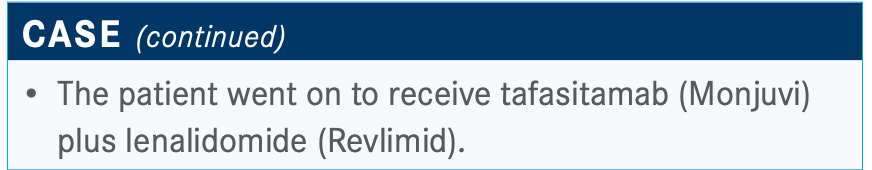
Tafasitamab and lenalidomide were approved in July 2020 for the treatment of DLBCL.2 It’s an interesting label in that it is approved for patients who are not transplant candidates, and so that raises the question of how you define a nontransplant candidate. It’s approved in combination withlenalidomide, 25 mg dosed 1 through 21 of a 28-day cycle; the lenalidomide is continued for a maximum of 12 cycles, but the tafasitamab is continued as monotherapy until disease progression or intolerance.
Tafasitamab was engineered for enhanced ADCC and direct cell death. Investigators saw encouraging activity in a phase 1 trial as a single agent. Then the rationale for combination with lenalidomide is because of the enhanced ADCC and because of activity seen with rituximab [Rituxan] and lenalidomide across a number of B-cell lymphoma subtypes. It was felt that this might be an interesting synergistic combination, and then [investigators] set out to explore it further in this phase 2 study in relapsed/refractory DLBCL.
Which trial looked at this combination, and what was the design?
The L-MIND study [NCT02399085] was an open-label, multi-center study.3 [Investigators] evaluated patients with relapsed/ refractory DLBCL. Now some important eligibility criteria are worth noting. They restricted eligibility to patients who had had 1 to 3 prior lines of therapy, so this is not a heavily pretreated patient population.
Patients who were ineligible for high-dose chemotherapy or autologous stem cell transplant were evaluated. There are not agreed-upon criteria for who’s not a transplant candidate, other than failing to have chemotherapy-sensitive disease. But because this [trial] would enroll patients who’d only had 1 prior line of therapy, that opens the discussion to how you would define a nontransplant candidate. This was done in a number of European sites where age alone is a factor, so generally patients over the age of 70 are deemed not appropriate candidates for stem cell transplant; it’s one of the more common criteria that were applied for defining this patient population.
The study schema outlined the dosing of lenalidomide at 25 mg [daily], which is standard in multiple myeloma studies. It’s a bit higher than the standard dosing done in most Hodgkin or non-Hodgkin lymphoma studies and speaks to the evolution of treatment over time, particularly when we’ve combined [lenalidomide] with other agents. Most of the time we’re starting at 20 mg, but for the purposes of this study, in the schema it was 25 mg of lenalidomide.
It’s also important to note that there was an induction phase with the combination, and particularly during cycle 1, tafasitamab was dosed weekly with an additional loading dose on day 4 of cycle 1 and then continued weekly up to all 3 cycles— so 12 weeks of treatment. Beyond cycle 3, it was dosed every other week or every 2 weeks until disease progression or intolerance. The primary end point of the study was objective response rate [ORR] as assessed by independent central review, and then key secondary end points included progression-free survival [PFS], duration of response [DOR], and overall survival [OS], in addition to safety.
There were 81 patients enrolled on the single-arm phase 2 study, and that speaks to the fact that lymphoma is a rare tumor type. The median age was 72, again [considering] that age over 70 was one of the most common criteria utilized to define a nontransplant candidate. About 51% of the patient population had an IPI risk score of 3 or higher, 75% had advanced-stage disease, median number of prior lines of therapy was 2, and primary refractory [disease] comprised only about 19% of the patient population. These patients generally were not primary refractory, though [the trial] did include some. Prior stem cell transplant patients might be a poor transplant candidate because they’ve already had transplant; [these patients comprised] about 11% of the patient population.
What were the efficacy data seen in the L-MIND study?
The ORR determined by the independent central review was quite notable. The ORR in patients with relapsed/refractory DLBCL was 60%, and the complete response rate was 43%. Probably even more important is that it appeared to be durable. The median DOR was 21.7 months. It was not reached among those patients who achieved a complete response, which was almost half the study population....DOR for patients who had a partial response [was markedly lower at] only 4.4 months, and 72% of [all] patients had an ongoing response beyond 12 months.
Importantly, there was a PFS in this patient population of 12.1 months, and median OS had not been reached. At 18 months, 64% of the patient population was still alive. I think this is important because if you put this into context, prior to the introduction of CAR T, if we look at the SCHOLAR-1 data—which were of a retrospective analysis of patients treated at MD Anderson Cancer Center, at Mayo Clinic, and in the Lysa group, which is a large French group— the median OS...was 6 months for patients with relapsed/ refractory DLBCL in second line or later.4 Again, this is a marked improvement over that.
The median PFS is also quite notable at 12 months [at 50%] because the median PFS for the CAR T population was only about 6 months. Now this probably reflects a specific patient population in that most of these patients were not as heavily pretreated as the CAR T population. A small percent- age were primary refractory.
Are other studies in the DLBCL setting looking at this regimen?
There were data reported at the 2020 American Society of Clinical Oncology Annual Meeting [from] the RE-MIND study [NCT04150328]....They essentially compared [the L-MIND] results with a synthetic control where they captured retrospective data of single-use lenalidomide in relapsed/refractory DLBCL and then tried to match that in terms of baseline characteristics.5
It looks like [the combination] was at least a significant improvement over lenalidomide monotherapy. Then the question is really: Is it better than the other options currently available in the relapsed DLBCL space? And that hasn’t been answered. It’s moving into front line. The phase 1b data were reported. There’s a randomized study that is launching, so that will then raise the question of how we sequence treatment in DLBCL.
What was the toxicity profile of tafasitamab and lenalidomide for these patients?
The most common adverse events [AEs] were neutropenia, anemia, and thrombocytopenia—not surprising to me because again this is an antibody in combination with lenalidomide.3 Grade 3 or higher neutropenia occurred in 48% of patients and grade 3 or higher thrombocytopenia in 17% of patients. Fortunately, febrile neutropenia was not high. There was 10% with grade 3 and 2% with grade 4. Growth factor use was at the discretion of the treating physician. It was not built into the protocol in terms of prophylactic use.
For the most common AEs that were nonhematologic, [what was noticeable was] the vast majority were grade 1/2, though about 9% of patients had a grade 3 rash, which is not unusual for lenalidomide in lymphoma. One percent had grade 3 diarrhea, and about 5% had hypokalemia. Some of that might be related to diarrhea and some nausea. Cough was about 1% at grade 3 or higher, and bronchitis was 1% at grade 4. Fatigue was another common AE, with 15% at grade 1 or 2.
Serious AEs occurred in 51% of the study population, although 19% were attributed to the study drug; 12% discontinued therapy as a result of toxicity, and then 9% had an AE of special interest. The AEs of special interest included tumor flare in 3 patients, and 1 patient with grade 2 basal cell carcinoma. Grade 3 [allergic dermatitis] occurred in 3 patients. There were 13% who had a treatment-emergent AE that led to death; however, according to the [investigators], none [of the deaths] were thought to be related to study treatment. The severity and incidence of the toxicities after lenalidomide was discontinued decreased, suggesting that a lot of the toxicity was due to the combination and not the CD19 monotherapy.
REFERENCES:
1. NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 4.2020. Accessed December 15, 2020. https://bit.ly/35H3YW0
2. FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. FDA. Updated August 3, 2020. Accessed December 15, 2020. https://bit.ly/34Emq2z
3. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
4. Crump M, Neelapu SS, Farooq U, et al. Outcomes in refractory diffuse large B-cell lymphoma: results from the international SCHOLAR-1 study. Blood. 2017;130(16):1800-1808. doi:10.1182/blood-2017-03-769620
5.Nowaskowski GS, Rodgers TD, Marino D, et al. RE-MIND study: a propensity score-based 1:1 matched comparison of tafasitamab + lenalido- mide (L-MIND) versus lenalidomide monotherapy (real-world data) in trans- plant-ineligible patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL). J Clin Oncol. 2020;38(suppl 15):8020. doi:10.1200/ JCO.2020.38.15_suppl.8020

Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen