Identifying New Biomarkers and Targets in Uterine Sarcomas
With expanding knowledge of the molecular characteristics of uterine sarcomas, investigators are working to develop treatments specific to each subtype.
As the shift toward precision medicine drives a push for more individualized treatments for patients with cancer, uterine sarcoma therapy is an area ripe for greater personalization. With expanding knowledge of the molecular characteristics of uterine sarcomas, investigators are working to develop treatments specific to each subtype.
Background
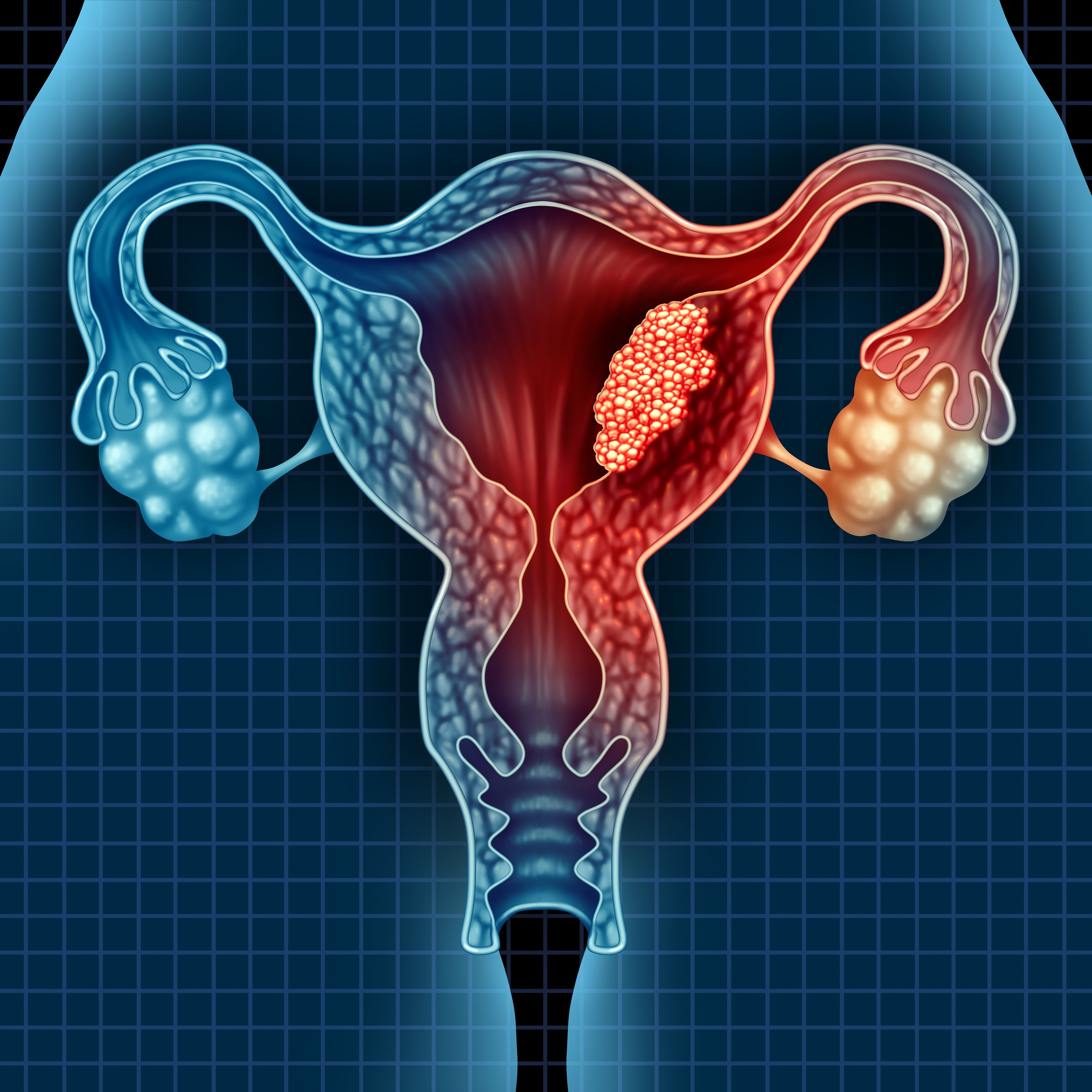
Uterine sarcomas are a group of rare, aggressive mesenchymal tumors, accounting for approximately 3% to 4% of all malignant uterine neoplasms.1-3 The most common histologic subtypes include uterine leiomyosarcoma (ULMS; 63%), endometrial stromal sarcoma (ESS; 21%), and undifferentiated uterine sarcoma (UUS; 5%). ESS is categorized as low or high grade (LG-ESS, HG-ESS).1,3 Carcinosarcomas were once considered part of the uterine sarcoma classification but are now considered and treated as high-grade epithelial tumors (carcinomas) instead. Uterine sarcomas of different histologic subtypes behave differently clinically, are often diagnosed postoperatively, can be difficult to differentiate from similar benign lesions, and carry varied prognoses depending on grade.4,5 These characteristics make uterine sarcomas a diagnostic and therapeutic challenge.
Suzanne George, MD, director of clinical research at the Sarcoma Center of Dana-Farber Cancer Institute, and Ravin Ratan, MD, MEd, associate professor in the Department of Sarcoma Medical Oncology at The University of Texas MD Anderson Cancer Center, discussed the difficulties and advancements in treating patients with uterine sarcomas in interviews with Targeted Therapies in OncologyTM. “Although uterine sarcomas may have a similar initial presentation,” stated George, “they behave biologically differently, spread differently, and respond to treatment differently. Inherently, they are different diseases.”
Ratan pointed out that uterine sarcomas are rare gynecologically, but they are somewhat common in the sarcoma space specifically and are likely more heterogeneous than currently believed. “If we consider HG-ESS, people may think it is a transformed version of LG-ESS, but it is actually a completely different process with a unique chromosomal translocation, making it a unique disease altogether.” These are just some of the characteristics of uterine sarcomas that make this group of cancers challenging to treat.
Current NCCN Treatment Guidelines
Hysterectomy with (or without) bilateral salpingooophorectomy is recommended for any operable uterine sarcoma, according to National Comprehensive Cancer Network (NCCN) guidelines.5 Testing for estrogen (ER) or progesterone (PR) hormone receptors is recommended to guide further therapy. However, George emphasized that “proper diagnosis is paramount and drives the treatment plan.”
Exact recommendations for adjuvant systemic therapy are not well defined given the heterogeneity of uterine sarcomas and lack of significant data; however, primary recommendations for high-grade uterine sarcomas include single-agent doxorubicin (Adriamycin) and combination gemcitabine (Gemzar) with docetaxel (Taxotere).5 In cases of ULMS, single-agent doxorubicin is active and less toxic than combination therapy. There are numerous secondary recommendations, including combination and single-agent therapies, depending on tumor type. Enrollment in a clinical trial is also highly recommended.
“The role of chemotherapy is typically for women who have developed recurrent or metastatic disease,” George said. However, Ratan mentioned that the absence of adjuvant recommendations is due to the lack of data, not the presence of negative data. “Over time there’s been recognition that a subset of patients with extremity and soft tissue sarcomas clearly benefit from chemotherapy based on their risk profile. I believe that’s likely true for ULMS as well, though we don’t have adjuvant trial data to parse treatment in the same way.”
Unfortunately, treatment for uterine sarcomas is not as guided compared with other neoplasms, in part due to the lack of data on appropriate biomarkers or targets for therapy.3 However, recent research may produce results that change that, and the latest NCCN guidelines highlight the importance of molecular features in addition to histopathologic criteria to better define each diagnosed tumor.5
Toward Precision Medicine
Diagnostic classification and prognosis have been improved with recent advances in our understanding of immunophenotypes and molecular characterization of uterine sarcomas. Characteristics of LG-ESS include positive ER and PR expression, an indolent disease course, and recurrent translocations involving JAZF1.2 A subset of HG-ESS tumors contain translocations resulting in a YWHAE-NUTM2A/B fusion and have an aggressive disease course, whereas others harbor BCOR alterations of unknown prognostic significance. Therefore, in high-grade sarcomas, testing for YWHAE and BCOR alterations may result in more precise diagnoses. However, ULMS lacks a single defining molecular abnormality; these tumors often exhibit multiple chromosomal changes.
Prospective Molecular Characterization
Investigators of a recent study (NCT01775072) evaluated tumors from 107 women with uterine sarcomas to determine whether prospective molecular characterization of advanced metastatic disease could indicate grade and/ or histological subtype-specific differences that would facilitate more accurate diagnosis and placement in clinical trials.2 Among the 80 patients with ULMS, the most common genetic changes were loss-of-function mutations in TP53 (56%), RB1 (51%), and ATRX (31%). Homozygous deletions of BRCA2 was identified in only 5% of these patients, and PTEN alterations were identified more in metastases vs primary samples. Low-grade tumors were found to have primarily silent genomes, whereas 50.5% of high-grade tumors exhibited whole-genome duplication. Genomic profiling influenced histologic diagnoses for 3 patients. Identification of actionable mutations led to matched targeted therapy for several patients, including several with somatically BRCA2-altered ULMS who showed evidence of clinical benefit from PARP inhibitors. The results of this study indicate that genomic profiling can improve diagnostic precision and treatment selection, but further research is needed to determine the true implications of these findings.
PLK4 in ULMS
A subset of ULMS cases were identified in recent genomic studies to have homologous recombination repair deficiency (HRD).6 PLK4 plays a key role in cell division by modulating centriole duplication, and PLK4 inhibition results in centriole dysregulation, increased double-strand DNA damage, mitotic catastrophe, and cell death.6,7
A recent preclinical study evaluated the PLK4 inhibitor CFI-400945 in wild-type cells and cell lines with gene knockouts generated using the CRISPR-Cas9 system.6 Plasmids encoding BRCA1- and BRCA2-targeting guide RNA, Cas9 protein, and selection markers were transfected into 2 ULMS cell lines, SK-UT- 1 and SKN, which were then treated with CFI-400945. The BRCA1- or BRCA2-deficient cells were more sensitive to the effect of PLK4 inhibition than the wild-type cells, including greater apoptosis and reduced viability.
“PLK4 [inhibition as cancer therapy] is an interesting hypothesis and could justify a phase 1 trial, but time will tell if it becomes a future therapeutic approach,” Ratan said.
SMOC2 as a Biomarker for ULMS
Preliminary data indicate that SMOC2, a secreted calcium-binding protein, is a potential biomarker for differentiating ULMS from its benign counterpart, uterine leiomyoma (ULM).8 Extracellular matrix (ECM) accumulation and remodeling are key for the development of ULMS and ULM. Expression of SMOC2, which is present in the ECM, is upregulated in ULM but downregulated in ULMS compared with normal myometrium. Additionally, the TGF-β1 pathway, which SMOC2 modulates to drive fibrosis, is down- regulated in ULMS and upregulated in ULM. These data are promising, given the challenges of differentiating ULMS from ULM, and further studies of SMOC2 are planned.
FOXP3+ T cells: A Positive Prognostic Indicator
A recent retrospective study characterized the tumor immune landscape, including full clinicopathological annotation, in 58 patients with uterine sarcomas.9 An overall prevalence of FOXP3-positive cells and protumor M2-like macrophages was identified. Four tumor type–independent immune signatures were identified, with infiltration of FOXP3-positive cells and M1-like macrophages associated with a favorable prognosis. Poor survival, upregulation of immunosuppressive markers and ECM-related genes and proteins, and YAP (an ECM signaling regulator) activation were associated with a high CD8-positive/ FOXP3-positive ratio in UUS and ESS. These findings indicate that uterine sarcomas pres-ent distinct immune signatures, independent of tumor type, which may have prognostic value. They also suggest ECM as a target for future treatments.
Ratan said using tumor-specific macrophages to achieve therapeutic response is not a new concept; however, clinical applications are lacking.
SATB2
SATB2 plays a role in altering gene expression by inducing chromatin remodeling.10 A recent study evaluated SATB2 protein expression in tissue sections from patients with a range of uterine tumors. With the cutoff for positive expression defined as at least 10% of tumor cells, the nuclear SATB2 score was negative in all endometrial stromal nodule samples (n=10) but positive in 83% of LG-ESS (n=29/35). Positive scores were also observed in 40% of UUS (n=4/10), 13% of ULMS (n = 2/16), and 14% of adenosarcoma sections (n=3/22). In ESS samples, nuclear SATB2 was associated with PR expression and decreased risk of disease-specific death in ESS (odds ratio, 0.06; 95% CI, 0.04- 0.81;P = .04). With a sensitivity of 83% for distinguishing between ESS and endometrial stromal nodules, SATB2 has potential as a diagnostic and prognostic biomarker.
Genetic Alterations as Potential Drug Targets
A recent analysis of tumor samples from 24 Chinese patients further illu-minated the varied landscape of genetic mutations in uterine sarcomas.11 The top 5 mutated genes in ULMS were TP53 (66.67%), ATRX (44.4%), RB1 (44.44%), BRCA2 (33.33%), and MED12 (33.33%). The fewest gene variations were identified in ESS, with 22.2% (2/9) of patients displaying mutations. Additionally, higher tumor mutational burdens was seen with carcinosarcomas compared with ULMS and ESS (P = .038). The study found that 70.83% (17/24) of enrolled patients (including those with carcinosarcoma) could benefit from targeted therapy or immunotherapy, based on mutations identi- fied in therapeutic target gene families such as CDK, PTEN, FGFR, BRCA, ATM, and NTRK.
Temozolomide + Olaparib for Advanced ULMS
The combination of temozolomide (Temodar) and olaparib (Lynparza) has produced promising initial results in patients with heavily pretreated ULMS.12 Single-agent temozolomide or olaparib showed limited activity in prelinical models of ULMS, though a case report revealed that a patient with BRCA2, TP53, and PTEN deletions was sensitive to olaparib monotherapy.13 National Cancer Institute (NCI) protocol #10250 (NCT03880019) is a single-arm, open-label, multicenter phase 2 trial. At a median follow-up of 10.8 months, the primary end point of objective response rate within 6 months of treatment initiation was 23% (5/22), the overall response rate was 27%, and tumor reduction was observed in 59% of patients. The median progression-free survival was 6.9 months (95% CI, 5.4 months-not estimable) and median duration of response was 12.0 months (95% CI, 9.5 months-not evaluable).12 The median overall survival was not yet evaluable. Analysis is ongoing, with correlative assays to evaluate the relationship between HRD or preserved SLFN11 expression (including intrinsic PARP inhibitor resistance) and sensitivity to the drug combination. A randomized trial is also planned.
Regarding the trial, George commented, “The results are encouraging and suggest the combinations hows some activity,and we look forward to follow-up studies with further evaluation in a larger patient population.”
Ratan hopes a follow-up study will include evaluation of HRD status. “The question is can you look at ULMS, assess the HRD status, then distinguish response based on that HRD status?” he asked.
Immune Checkpoint Inhibition
Responses to immune checkpoint inhibition have been varied in case reports thus far, even though immunotherapy has been approved for the treatment of microsatellite instability–high tumors. The NCCN guidelines list pembrolizumab (Keytruda) as a secondary, biomarker-directed systemic option in the second-line setting for patients with uterine sarcomas who have tumor mutational burden–high tumors.5,14
For example, in a trial of patients with ULMS who were treated with pembrolizumab, the majority of patients progressed early on.14 However, 2 case reports have described individual responses to the drug, with 1 patient achieving a complete remission lasting for more than 2 years.
Potential mechanisms of resistance to immune checkpoint inhibitors include loss of PTEN, loss of neoantigen expression, and the presence of high numbers of regulatory T cells.15
Looking Forward
“Uterine sarcomas remain a group of distinct diseases that vary biologically and can be uniquely treated depending on the underlying molecular alterations, and there are many patients who lack therapeutic targets and require standard cytotoxic chemotherapy,” George stated. She went on to emphasize the need to identify which patients will respond. “I believe the potential opportunity is greatest with combination therapy, and the continued observation of DNA damage repair vulnerabilities provides potential for therapeutic investigation.”
Ratan explained that immune therapies have not been effective in ULMS, which is associated with an immune-inhibitory environment that can hopefully be overcome in the future. In terms of the future, he said, “The most promising avenue is looking to target specific changes in these tumors, and the most clinically relevant approach currently is evaluating BRCA[-mutated] and HRD tumors.” He pointed out that in other cancers, such as breast and ovarian, PARP inhibitors can be beneficial and the use of a DNA-damaging agent makes sense; however, the data in the uterine sarcoma space are currently insufficient.
George mentioned the FDA’s recent approval of nab-sirolimus (Fyarro) for the treatment of patients with locally advanced, unresectable, or metastatic malignant perivascular epithelioid cell tumor (PEComa).16 Approximately one-fourth of the patients in the phase 2 AMPECT trial (NCT02494570), on which the FDA based its approval, had a diagnosis of PEComa of the uterus, and investigators observed a 39% overall response rate (95% CI, 22%-58%) in the overall cohort. The median progression-free survival was 10.6 months (95% CI, 5.5-not reached [NR]) and the median overall survival was 40.8 months (95% CI, 22.2-NR). After a median follow-up of 2.5 years, the median duration of response had still not been reached.17
“[Although] these are rare, there are certain subtypes that have very unique and effective therapies we need to make sure we’re aware of,” George said. She went on to explain how the variety and rarity of these diseases calls for further collaboration to improve research progress moving forward, and she described a grant awarded by the NCI to the nonprofit Count Me In initiative and the Broad Institute of the Massachusetts Institute of Technology and Harvard. Collaborative research in ULMS will be supported, with the goal of achieving discoveries in the genomic roots of cancer, mechanisms of therapeutic resistance, and potential treatment strategies.18
REFERENCES
1. Eiriz I, Vitorino M, Gomes F, Braga S. Uterine sarcomas: a retrospec- tive analysis of a cohort of 62 patients. Cureus. 2021;13(2):e13349. doi:10.7759/cureus.13349
2. Hensley ML, Chavan SS, Solit DB, et al. Genomic landscape of uterine sarcomas defined through prospective clinical sequencing. Clin Cancer Res. 2020;26(14):3881-3888. doi:10.1158/1078-0432. CCR-19-3959
3. Abu-Rustum NR, Yashar CM, Bradley K, et al. NCCN Guidelines insights: uterine neoplasms, version 3.2021. J Natl Compr Canc Netw. 2021;19(8):888-895. doi:10.6004/jnccn.2021.0038
4. Desar IME, Ottevanger PB, Benson C, van der Graaf WTA. Sys- temic treatment in adult uterine sarcomas. Crit Rev Oncol Hematol. 2018;122:10-20. doi:10.1016/j.critrevonc.2017.12.009
5. NCCN. Clinical Practice Guidelines in Oncology. Uterine neoplasms, version 1.2022. Accessed April 22, 2022. https://bit.ly/3ya6F2w
6. Chong TY, Lee HHY, Yam JWP, et al. Uterine leiomyosarcoma with homologous recombination deficiency is highly sensitive to polo-like kinase 4 inhibitor. Poster presented at: American Association for Cancer Research Annual Meeting 2022; April 8-13, 2022; New Orleans, LA. Abstract 5394. https://bit.ly/3LDqC5A
7. Zhang X, Wei C, Liang H, Han L. Polo-like kinase 4’s critical role in cancer development and strategies for Plk4-targeted therapy. Front Oncol. 2021;11:587554. doi:10.3389/fonc.2021.587554
8. Cai C, Falcao R, Kokaraki G, et al. SMOC2 as a potential biomarker with diagnostic value in uterine leiomyosarcoma. Poster presented at: American Association for Cancer Research Annual Meeting 2022;April 8-13, 2022; New Orleans, LA. Abstract 5005. https://bit.ly/38D8fPz
9. Gultekin O, Gonzalez-Molina J, Hardell E, et al. FOXP3+ T cells in uterine sarcomas are associated with favorable prognosis, low ex-tracellular matrix expression and reduced YAP activation. NPJ Precis Oncol. 2021;5(1):97. doi:10.1038/s41698-021-00236-6
10. Le Page C, Almadani N, Turashvili G, et al. SATB2 expression in uterine sarcoma: a multicenter retrospective study. Int J Gynecol Pathol. 2021;40(5):487-494. doi:10.1097/PGP.0000000000000730
11. Xue F, Wang Y, Xu Z, Wang F, You D. 806P Genomic alteration char- acteristics and potential drug targets of uterine sarcoma. Ann Oncol. 2021;32(suppl 5):S764-S765. doi:10.1016/j.annonc.2021.08.1248
12. Ingham M, Allred JB, Gano K, et al. NCI protocol 10250: A phase II study of temozolomide and olaparib for the treatment of advanced uterine leiomyosarcoma. J Clin Oncol. 2021;39(suppl 15):11506- 11506. doi:10.1200/JCO.2021.39.15_suppl.11506
13. Pan M, Ganjoo K, Karam A. Rapid response of a BRCA2/TP53/ PTEN-deleted metastatic uterine leiomyosarcoma to olaparib: a case report. Perm J. 2021;25:20.251. doi:10.7812/TPP/20.251
14. Wang YJ, Williams HR, Brzezinska BN, et al. Use of pembrolizum- ab in MSI-high uterine leiomyosarcoma; a case report and review of the literature. Gynecol Oncol Rep. 2021;35:100701. doi:10.1016/ j.gore.2021.100701
15. De Wispelaere W, Annibali D, Tuyaerts S, Lambrechts D, Amant F. Resistance to immune checkpoint blockade in uterine leiomyosar- coma: what can we learn from other cancer types? Cancers (Basel). 2021;13(9):2040. doi:10.3390/cancers13092040
16. FDA approves sirolimus protein-bound particles for malignant perivascular epithelioid cell tumor. FDA. Updated November 23, 2021. Accessed April 22, 2022. https://bit.ly/3LmkdeM
17. Wagner AJ, Ravi V, Riedel RF, et al. nab-sirolimus for patients with malignant perivascular epithelioid cell tumors. J Clin Oncol. 2021;39(33):3660-3670. doi:10.1200/JCO.21.01728
18. Dana-Farber, Broad Institute and Count Me In receive $16 million grant to launch patient-partnered research initiatives in rare cancers. News release. Dana-Farber Cancer Institute. February 17, 2021. Accessed April 22, 2022. https://bit.ly/3xH8EuS

Advances in Subsequent Therapies Shake Up Sequencing of ccRCC Treatment
April 25th 2024With the approval of belzutifan and other newer data for treating patients with recurrent renal cell carcinoma, the state of subsequent therapies is advancing beyond the reuse of frontline options with impacts on duration of response and quality of life.
Read More
Ornstein Advises on Starting Dose and Management of Lenvatinib in RCC
April 21st 2024During a Case-Based Roundtable® event, Moshe Ornstein, MD, MA, provided guidance on dosing and toxicity concerns in a patient treated with lenvatinib plus pembrolizumab for advanced renal cell carcinoma.
Read More