Roundtable Discussion: Participants Evaluate the Use of Transplant and MRD in Newly Diagnosed Multiple Myeloma
During a Targeted Oncology Case-Based Roundtable event, Clifton C. Mo, MD, discussed the treatment of newly-diagnoses multiple myeloma.
Clifton C. Mo, MD

During a Targeted Oncology Case-Based Roundtable event, Clifton C. Mo, MD, assistant professor of Medicine, Harvard Medical School Director of Autologous Stem Cell Transplantation for Multiple Myeloma, Jerome Lipper Multiple Myeloma Center, and LeBow Institute for Myeloma Therapeutics at Dana-Farber Cancer Institute, discussed the treatment of newly-diagnoses multiple myeloma.

MO: Tell us how you have the initial conversation with your patients with newly diagnosed multiple myeloma [NDMM] regarding long-term prognosis and outcome.
ILYAS: For a transplant-eligible patient, I typically start with the available treatment strategies, including the initial induction systemic chemotherapy options. I discuss the transplant option, whether that would be early or delayed. I would definitely ask my patient to see a transplant team which, being in Maine, [would typically mean at] our preferred center, Dana-Farber Cancer Center. From the get-go, I will get the patients in to have that discussion as well.
As far as the prognosis, in the absence of any high-risk features I tell them that the likelihood [of putting] this disease in remission, and the long-term prognosis, is extremely good. I will also add that not only is the initial treatment option [good, but that] in the event of relapse, we also have extremely effective treatment strategies…that have very favorable outcomes in that setting.
COLVIN: It’s still a terminal disease, so you have to start with that and tell them it’s terminal. I talk about the average survival. The Mayo Clinic published [a review of patients with NDMM], from 1985 to 1998, [showing that] average survival was only 2 years.1 I don’t know where we are now—are we at 6 years…9 years? But you have to start from the beginning, that we’re dealing with a terminal condition that has no cure.
ILYAS: That’s correct, but in terms of the life expectancy I don’t think we know exactly. I just make clear that this is not a curable disease but a highly treatable disease. No question about it. ASIK: What about cytogenetics for the prognosis, cytogenetics to define prognosis for the MM outcome? Defining young patients is all about performance status rather than age or comorbid conditions, I would say.
NEWSOME: As far as prognosis, I generally let them know it’s technically not a curable disease [but that] it’s very treatable. I always warn them about going online and reading median survivals from 15 years ago, because clearly, over the past 10 or 15 years, we’ve had an explosion of treatment options [and longer] median survivals. I let them know it’s not a curable disease [but that] we have many, many treatment options both in the first line as well as subsequent lines. Certainly the prognosis has changed.
MO: I agree. In fact I try to tell patients essentially verbatim what you just said. I find it interesting that on the one hand, [with Dr Ilyas], we have a real focus on optimism and the possibility for a good long-term outcome, and [with] Dr Colvin [we have] the desire to focus on being grounded in reality and the fact that this is incurable and is not associated with a normal life expectancy. I completely agree with you both, and I try to walk the fine line between telling the patient what they need to hear, in terms of this being an incurable disease and something that has, at least historically, been associated with a very poor prognosis. We all see patients who still do poorly with MM and don’t survive for more than a few…years.
However, I also like to stress that it’s a rapidly changing field, that we’ve gone from 0 FDA-approved drugs in 2003 to 15 as of [recently]. I think we can confidently say that, overall, we’re seeing a doubling of overall survival [OS] based on data that have been available for just short of a decade. With all these newer drugs, it’s impossible to tell. That’s how I approach it. We owe it to patients to tell them they have something that is very serious and, at least historically, [has a] very poor prognosis, but [in a way that is] appropriately peppered with optimism.
The second question is how do we define who is young. Is there a magic number we have in our heads, or not so much?
ROZELL: I wouldn’t say there’s necessarily a magic number. You see 70- and 80-year-olds who look extremely healthy, very fit, and then you can see 50-year-olds who seem like they’re 100. So I think it’s really more based on their performance status and comorbidities rather than an age.
MO: Increasingly, we’re recognizing that age really is just a number, and you can have a very robust patient in their mid to late 70s and a very frail 50-year-old. Just of note, we now have multiple frailty indices and there’s an International Myeloma Working Group frailty score that can be used now, [which is] being studied. So I think it’s much more of a fluid spectrum rather than a strict cutoff. At least historically, in Europe, for example, with the initial transplant studies it was a pretty defined cutoff of age less than 65 [years]. In the United States, …less of a fine line has been drawn. There are plenty of patients in their 70s, as well as patients even in their late 70s, who are still [receiving transplants] at some centers and, I think, safely.
GORUSU: I agree with [Dr Mo’s] comment. When we say “defining young,” the thing that would come to my mind is, is it because I’m looking at the transplant that I’m going to offer—chimeric antigen receptor [CAR] T-cell therapy—or is it the steroid dose. I think when we are assessing the age of the patient to define the appropriateness, it’s going to change [depending on what] you’re considering them for, [including] the different lines of treatment, the medical management, transplant, or some other kind of CAR T-cell–based therapy. I have to only imagine that these eligibility criteria will be a little bit fine-tuned by the type of treatment you’re offering to your patient.
MO: I completely agree. In general, when we start off with a patient with NDMM, there are 2 [thoughts]: number 1, which induction regimen are we going to use, and number 2, is this patient going to transplant or even going to be considered for a delayed transplant.
KATOCH: What would you tell a patient [with standard-risk stage II MM]? What is a transplant-eligible patient’s prognosis in terms of how many years, if the patient were to pin you down?
MO: In 2021 I think it’s an impossible question to accurately answer because of all the new types of therapies that are either coming down the pike or already in our pharmacies. What I would say is that for a young patient who’s transplant eligible, in 2021, with standard-risk disease without high-risk cytogenetic features or multiple high-risk cytogenetic features, …survival of greater than a decade is a very realistic possibility. With everything new that’s coming down the pike, our goal is to try to measure this patient’s survival in terms of decades, which I think is a realistic goal, knowing that that’s far from a guarantee that they’re going to get there. I think it is now a realistic goal, whereas a decade ago, much less 2 decades ago, I wouldn’t [have said] that.
I’m not able to throw a number down on the table. I wish that I [could], but I think we’re now in this Wild West, so to speak, where the treatment landscape is advancing so rapidly that we just don’t know. But what we do know is that it’s continuing to improve, year over year, based on all the new therapies and the new mechanisms of action that we have at our disposal now.
With high-risk patients, I have a bit more of a guarded discussion. I still think it’s realistic to get a high-risk patient over a decade of survival, but it’s by no means a guarantee.
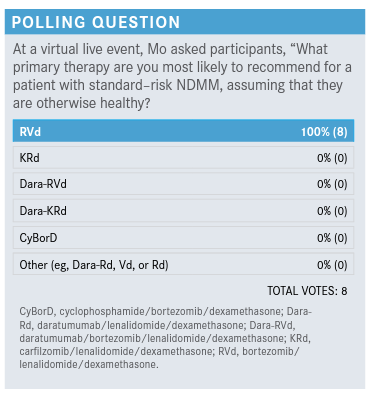
MO: It’s unanimous. Everyone here would pick the RVd triplet. I’m voting as well, so I also picked that, but I was expecting to see a little bit more of a smattering. Really interesting that we’re all in agreement there.
YUN: When I get a patient with MM, I first assess the cytogenetics and performance status and whether they’re transplant eligible. For primary therapy, my goal is first to refer them to Dana-Farber or some tertiary care center where transplant is feasible, because we are at a small community hospital where we don’t do transplants. If they’re high risk, I would tend to start with carfilzomib [Kyprolis] triplet therapy and maybe add on daratumumab [Darzalex]. For the standard-risk patient, I would tend to stick with RVd [lenalidomide (Revlimid)/bortezomib (Velcade)/dexamethasone]. If they have kidney failure, [I would] probably start off with CyBorD [cyclophosphamide/bortezomib/dexamethasone]. If they’re frail and elderly, I would use doublet with lenalidomide/dexamethasone. That’s usually what I think about.
MO: In terms of your choice of KRd [carfilzomib/lenalidomide/dexamethasone], is that based on the demonstrated potency of the drug in the relapse setting and then bortezomib-refractory patients…[making] you reach for carfilzomib over bortezomib?
YUN: In terms of the cytogenetics, if I consider them high risk, I want to [treat them] as best I can, and I think carfilzomib might be superior to bortezomib in that respect.
MO: I can tell you’re far from alone in that suspicion, that there may be a role for or an advantage to carfilzomib, specifically in high-risk patients. Has anyone given a doublet, lenalidomide/dexamethasone, alone to a 50-year-old patient in the past couple of years or is that uncommon these days?
ILYAS: For those patients with high risk, I think it still might be reasonable to try a 3-drug regimen, RVd. [Then], after a couple of cycles, restage based on their response, whether or not adding the 4-drug regimen can be done as well.
MO: Which proportion of our patients with NDMM, who are young and fit, do we think are transplant eligible: 30%, 50%, 60%, 70%?
GORUSU: My guess would be 40%.
KATOCH: Where I practice, I would say about 50% to 60% seem to be transplant eligible.
MO: I know that it all comes down to what one’s definition of transplant eligibility is. As I’m sure it’s a surprise to no one, that may differ depending on whom you ask, and maybe on what center you go to. I’ll tell you that, in general, we fairly rarely perform transplants in patients older than 75 years at Dana-Farber. Not to say we never do—that’s not a line in the sand, so to speak—but that’s the age at which we start to get increasingly nervous in terms of frailty and eligibility. But then the other piece of this puzzle is necessity. With all these other options we have, with these highly potent induction regimens we have now that we didn’t have 10 years ago, and with all these new immunotherapy options coming down the pike, even if we could safely perform a transplant in a 78-year-old, is that necessarily in the patient’s best interest anymore?
But as the median [age] at time of diagnosis is mid to late 60s, by definition we have a lot of our patients who will be considered transplant ineligible. Interestingly, a lot of those patients will not be referred for a transplant eligibility consultation. The statistics show that the majority of patients in that age range, or at least a lot of them, won’t even get an initial consultation. So I would always encourage [consultation] if there’s any question at all regarding eligibility.
MO: What do people think about early vs delayed transplant? What do people think about triplets vs quadruplets, and KRd vs RVd? And last but not least, how strongly do we feel about minimal residual disease [MRD] as an important thing to be incorporating into our treatment decisions?
GORUSU: I think the MRD data are so tempting [when it comes to making] the treatment decisions…but I’ll be cautious in which patients I prefer to take that quadruplet. It makes sense, but I need a little bit more data to assure me that I’m not basing my decisions on assumptions.
MO: I think I’m the same way. Does anybody else feel the same, or differently, about MRD? Is anybody using MRD?
COLVIN: I’m not currently using that outside of a clinical trial.
KATOCH: Me neither.
NEWSOME: No, I haven’t been using it either. I don’t generally get bone marrow tests for people unless I’m worried they have significant residual disease.
MO: I think I’m with everyone in the group. I agree wholeheartedly that it’s very tempting whenever we see studies showing that MRD is significantly correlated with progression-free survival or even OS. Looking at the data retrospectively, it’s very tempting to say it’s the next thing.
I think there’s a decent chance that we may be at the cusp of transitioning from the triplet to the quadruplet era, but importantly, we just don’t have longer-term data. We don’t have a phase 3 study demonstrating OS advantage, which I think would still be the gold standard in saying that this is the absolute, new, no-questions-asked standard of care. I think we may get there, but we’re just not there yet. In practice, I support the use of a daratumumab [dara]-based quadruplet, either dara-RVd or even dara-KRd.
In terms of using MRD to guide therapy, what we don’t yet have [are data from] studies that escalate therapy, or de-escalate therapy, based on MRD status. Those studies are ongoing, but we don’t have [the information] yet. For high-risk patients, I tend to support, sometimes even suggest, strong consideration of dara-RVd in the absence of long-term data, just because these are the patients we’re most worried about. They have a high chance of not doing well. Then with standard-risk patients, I have the discussion of potential benefit, but it’s a less strong recommendation. That’s where I’m at in terms of MRD, as well as quadruplet vs triplet therapy.
KATOCH: If a patient today asks you, “Should I go for a transplant? Is it going to make me live longer and by how much?” what do you say to that?
MO: This is a conversation I have probably 5 to 6 times a week. What I say is that transplant has historically, for over 2 decades, been the standard of care based on convincing data showing an OS advantage to high-dose chemotherapy vs standard chemotherapy alone. But the added advantage of an early transplant, a transplant at first remission, is unquestionably less [evident] than it was in 1996.
There definitely are still advantages to early transplant, [however]. The main advantage, which is a significant one—the degree of significance is debatable—is that we definitely still see a progression-free survival advantage. I tell my patients that there’s a significantly higher likelihood they’re going to stay in their first remission longer by doing a transplant in first remission than by going with the delayed approach.
We’re in a situation now where there are pros and cons to early transplant and pros and cons to late transplant. I tend to run late in my clinic and my patients tend to get different levels of annoyed with me because I have very long conversations. At the end of the visits, I’d like to think that most patients are well informed and…already at least starting to tell me which way they’re trending. I think the personal preference of the well-informed patient is of utmost importance in 2021 when making the transplant decision.
It’s very tempting for me to throw everything but the kitchen sink at a high-risk patient up front, meaning to do a transplant right off the bat if they’re high risk. [But] I don’t think we have the data to say that that actually improves OS in high-risk patients. It’s a very complicated discussion. I don’t mean to give a cop-out answer, but… the right answer can be very different between 2 different patients these days.
KATOCH: The problem is that these patients go see transplanters, they get all this information, and they’re so confused. Then they come back and they want us to make the decision for them. I want to be able to tell them something that makes sense. All of them say, “Why should I do that? If you already have drugs that are going to keep me in remission, why do I have to put myself through that?”
MO: Well, just to play devil’s advocate, one of the arguments for still doing early transplant, other than the progression-free survival advantage, is we do see significantly higher rates of MRD negativity [when] we transplant, and we know there’s an association between MRD negativity and OS. Does that mean, on an individual basis, we should be giving everyone a transplant in the face of the long-term data? I don’t think so, but that is an argument that’s made.
My general approach is to try to not put everything on [community physicians]. I tend to see patients around [the time] when they first get started or a month after they start treatment, and I basically schedule a follow-up visit— even a Zoom visit—after about 3 to 4 months of induction. During those 3 to 4 months, I say, “Sleep on it, talk about it with your family, talk about it with [your physician], and then we’ll decide at month 4.” That’s when I generally target either the transplant or the stem cell collection, somewhere after 6 to 9 months of therapy. If we wait an entire year to a year and a half to collect cells, then we may run into increasing problems with mobilization failure and collecting enough cells. But I don’t think there’s an immediate rush to make that transplant decision right out of the gate. In fact, I think that’s probably not the right answer because a lot of it is also dependent on how the patient does, how the patient tolerates therapy.
We talk a lot about high risk vs standard risk, but there’s also functional risk. We’ve all had patients who have no high-risk cytogenetics and then after 6 months of RVd they’re still in a partial response. So that’s why I think the transplant decision should be methodical and not necessarily rushed into.
ILYAS: Are there any patients who, after the decision of delayed transplant after whatever reason—some events or intercurrent illnesses—will become ineligible for transplant in the future? Have you come up with any scenario like that?
MO: Admittedly that is a very real risk of not doing a transplant in first remission.…There is a risk that the disease may not be well controlled enough. I don’t think that’s as much of a risk in 2021 as it was 10 years or even 5 years ago. Because now that we have daratumumab, now that we have all these other, newer agents, …it’s increasingly unlikely that we can’t get a patient to a transplant in second remission. But it is a possibility. Then of course, the second possibility is, say somebody had their stem cells collected, they’re doing fine, and then a year later they have a myocardial infarction and now they have heart failure. Then their myeloma relapses and now we say, “We have your cells, but you’re no longer transplant eligible.” That is a risk I definitely make sure the patient’s aware of when making the decision.
Reference:
1. Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21-33. doi:10.4065/78.1.21
KATOCH: The problem is that these patients go see transplanters, they get all this information, and they’re so confused. Then they come back and they want us to make the decision for them. I want to be able to tell them something that makes sense. All of them say, “Why should I do that? If you already have drugs that are going to keep me in remission, why do I have to put myself through that?”
MO: Well, just to play devil’s advocate, one of the arguments for still doing early transplant, other than the progression-free survival advantage, is we do see significantly higher rates of MRD negativity [when] we transplant, and we know there’s an association between MRD negativity and OS. Does that mean, on an individual basis, we should be giving everyone a transplant in the face of the long-term data? I don’t think so, but that is an argument that’s made.

CAR T and CRS Adverse Events Considered in Relapsed Multiple Myeloma
October 24th 2024During a Case-Based Roundtable® event, Saad Z. Usmani, MD, FACP, MBA, discussed CAR T-cell therapy as third-line therapy for a patient with relapsed/refractory multiple myeloma and relevance of the KarMMa-3 trial for their treatment.
Read More