Skin Cancer Awareness Month: TILs Offer New Hope in Advanced Melanoma
Jose Lutzky, MD, discussed the promise of tumor infiltrating lymphocyte therapy for difficult-to-treat advanced melanoma.
Tumor infiltrating lymphocytes and oncolytic adenovirus TILT-123 for patients with metastatic malignant melanoma
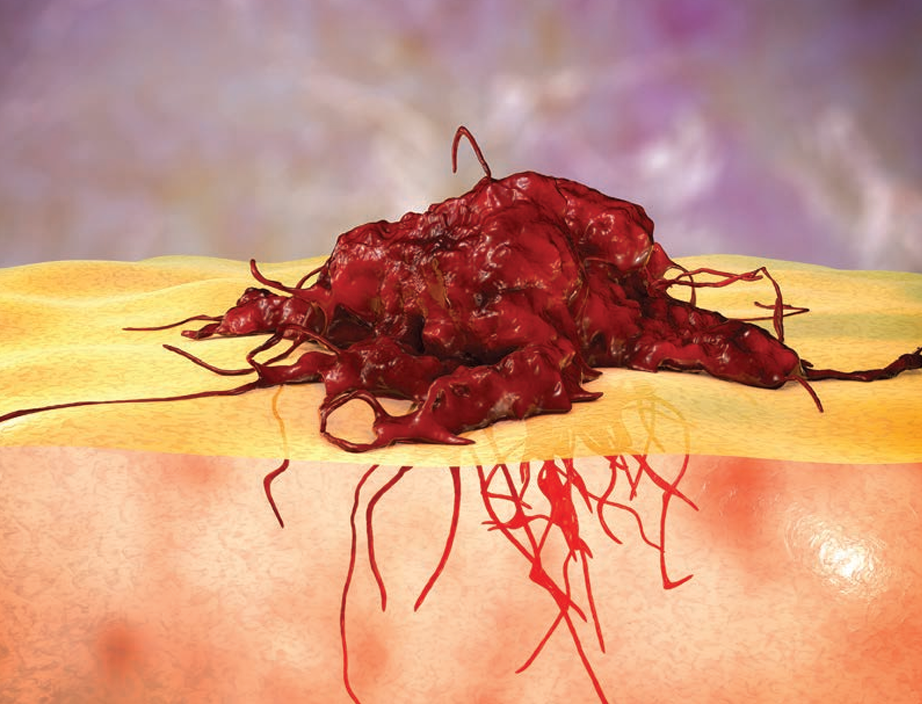
In February 2024, the FDA approved lifileucel (LN-44), a tumor infiltrating lymphocyte (TIL) therapy for advanced melanoma. This is the first of its kind for solid tumors and represents a significant step forward for melanoma treatment.
TIL therapy harnesses a patient's own immune system to fight cancer. Doctors extract immune cells from a patient's tumor, grow them in a lab, and then reinfuse them back into the patient. These TILs are specifically targeted to fight the patient's unique cancer cells.
This therapy is particularly promising for patients whose melanoma has not responded to other treatments like checkpoint inhibitors or targeted therapy. Studies have shown a 32% response rate among patients who received TIL therapy, and over half of those who responded maintained that response for more than 3 years.
Jose Lutzky, MD, a skin cancer physician at Sylvester Comprehensive Cancer Center, emphasized the significance of TIL therapy as it offers a new option for patients with limited treatment choices and builds upon the success of previous immunotherapies in melanoma. Sylvester is also participating in a clinical trial to further improve TIL therapy by genetically modifying the immune cells to enhance their effectiveness.
While TIL therapy offers great promise, it is not without challenges. The treatment process can be demanding, involving surgery, chemotherapy, and post infusion treatments. However, the potential benefits outweigh the difficulties for many patients.
The approval of TIL therapy marks a new era in melanoma treatment, offering hope for patients with advanced disease. In an interview with Targeted Oncology, Lutzky, director of cutaneous oncology, medical director of the Clinical Trials Coordination Unit, and cutaneous and ocular oncology site disease group lead, discussed TIL therapy in melanoma and a study (NCT05361174) taking place at Sylvester Comprehensive Cancer Center looking at a modified TIL option.
Jose Lutzky, MD

Targeted Oncology: What does the current treatment landscape in metastatic or advanced melanoma look like?
Lutzky: They cannot be treated by surgery, or it has spread widely. We divide them usually in 2 different types: melanomas that have a BRAF mutation and others that do not have a BRAF mutation. We tend to start both types of melanoma treatment with checkpoint inhibitors drugs like ipilimumab [Yervoy], nivolumab [Opdivo], pembrolizumab [Keytruda]. A new [option] is a combination of nivolumab and relatlimab that is branded Opdualag. That usually can control about half of these patients, and usually for a long period of time. But there is this other half that either does not respond to treatment from the get-go, or they respond and then they become resistant or refractory to treatment. Those patients are the most difficult patients to handle. There is also a group of patients that respond but develop significant immune-related adverse events that we cannot treat very easily.
How are TILs used in melanoma? How do they vary from the standard of care?
Right now, that treatment is focusing on this group of patients are either refractory or resistant, and we try a bunch of other things. We try oncolytic therapy, we try different drugs, different ways to try to restore sensitivity to checkpoint inhibitors. TIL therapy is a form of cell therapy which is infusing immune cells into patients hoping that there are enough of those immune cells there are going to attack certain proteins or antigens in the tumors. This is not new at all. The concept has been around for 30 years. In fact, the first TIL therapy for melanoma was in, I believe, 2005, from the group at the [National Institute of Health (NIH)]. They had been studying that for a long time and had a bunch of models that suggested that that might work, and it did work in a number of patients.
The problem is that the process was very complex, and that there was there were only a few centers in the country that could do that. It took a long time. In many instances, by the time that they were able to have the cells ready for a patient, the patient was no longer around. More recently, a number of companies, particularly the one that got the [FDA] approval, decided that they wanted to make this available to more people and confirm the results that the NIH had years ago. They created a facility to produce these cells in the US and 1 in Europe and had a number of cancer centers that had interest and expertise in cell therapy put together this trial.
Eventually, the trial showed that, for patients that were refractory and resistant to checkpoint inhibitors and for patients that have a BRAF mutation that can be treated with BRAF inhibitors and MEK inhibitors, that those patients have failed those treatments, that group of patients ended up with about a 30% response rate. The interesting thing and important thing about this also is that these responses were durable. Once [a patient] responds, those responses can last. The median time has not been reached yet. But those patients that respond have been responding for over 3 years now.
How does the process work?
The idea here is that the immune system is trying to fight the tumor, and it loses the battle, and that's why the tumor is growing. When you look at the tumor, there are cells in that tumor microenvironment that are there to kill the tumor. But there are a number of cells that are opposing that, including some of the T lymphocytes, that actually are immunosuppressive regulatory T cells.
The idea was to take a piece of the tumor, pull out the T lymphocytes that are targeting the tumor, and they are trying to kill the tumor and take them away from that suppressive environment in the tumor, grow them in culture in large numbers, and then give them back to the patient. But to give them back to the patient, you would want to get rid of immunosuppressive environment that is in the tumor, so patients get what is called lymphodepletion, which is chemotherapy that will kill all of those cells that. Then immediately after that, you give back the cells. Patients, at this point, have to be in the hospital, because in order to activate the cells, [we] have to give a drug called interleukin-2 in high doses, and that treatment has a lot of [adverse] effects that are temporary, but pretty intense, and patients have to be in the hospital for that.
Could you provide some background on the study taking place at Sylvester Comprehensive Cancer Center and what is being investigated?
The kind of TIL that was approved now is untreated or unmodified. There are a number of studies now that are modifying these T cells to make them more active against the tumor. Also, there are other studies that are trying to modify the cells to make them less susceptible to these immune suppressive mechanisms.
One of the immune suppressive mechanisms is that tumors express this protein called PD-L1, which attaches to a receptor in the T-cell called the PD-1 receptor. When that happens, it neutralizes the T-cell. Imagine a cell holding a knife that only fits in a certain place in the tumor cell. The idea here was to knock out this receptor from the T cells so this PD-1 could not neutralize them anymore.
In this study that we are doing, the process is exactly the same as I mentioned before: You take the cells out, but when you take the cells out of the tumor after surgery, you modify those cells. You knock out this receptor, the PD-L1 molecular weapon methods, and then when you have those TILs that do not have the PD-1 receptor, then you expand them, you freeze them, and then you give them back when the patient is ready after lymphodepletion. The idea is that it might be more effective because you're minimizing 1 of the mechanisms by which the tumors do not respond to immunotherapy.
What is the importance of doing this study in Florida?
Florida has the second highest incidence of melanoma in the country after California. It is a big problem here. Trying to get the other 50% of patients into a durable response is the objective. We can salvage 30% with this treatment that is already approved, and not even that because remember, not everybody is a candidate for regular TILs because [the patient has] to be in good shape [and] have the appropriate performance status to be a candidate. There is a long way to go here. That is the objective of trying and we are always trying to get better. We have a number of other T-cell therapies in which we are modifying the T cells with different in different ways to target different antigens. But in terms of tumor infiltrating lymphocytes, that is what we're doing. I think it is an important trial. We will see how it pans out.
Is there any other research happening with TILs or advanced melanoma that clinicians should be aware of?
We have a pretty robust clinical research program for melanoma. We have a couple of trials in which we are modifying the T cells to be more targeted. One of the problems with this approach is that when we do that, patients have to have a specific type of immune system or so-called HLA type. Sometimes, the HLA type that we target, it reaches only sometimes 40% to 50% of the population. We are doing other trials now that are targeting other HLA types to try to offer this to more people.
We are also doing trials with modified cytokines. Interleukin-2, when used by itself, has a response rate of about 10% in metastatic melanoma, and about 6% of the patients get a complete response, and the tumor never comes back. It was used in the past a lot because of that 6% response. But as I mentioned, it is a very toxic drug. When checkpoint inhibitors came along, we stopped using interleukin-2. Interleukin-2 helps kill the tumor cell, but also increases some of these inhibitory cells. Scientists have defined which receptors do what, in terms of the good effects and the bad effects. There are now a number of studies out there that modify the interleukin-2 molecule to only do the good things and less of the bad things.
That particular study that we are using has an antibody attached to the interleukin-2 molecule that brings it only to the CD8 cells, which are the lymphocytes, that are the soldiers of the immune system and go after the tumors. That approach has had less toxicity. Patients do not need to be in a hospital for that, and we have already seen some responses.
We have a number of oncolytic viral therapies which are either given directly into the tumor or into the bloodstream. In these approaches, the idea there is to sensitize tumors that are not responding to immunotherapy. There are so called cold tumors, meaning they do not allow the immune cells to infiltrate the tumor.
Cretostimogene Grenadenorepvec Shows High CR Rate in BCG-Unresponsive NMIBC
July 17th 2024Mark D. Tyson, II, MD, MPH, discussed treatment with cretostimogene grenadenorepvec in high-risk Bacillus Calmette-Guérin-unresponsive non-muscle invasive bladder cancer with carcinoma in situ and data from the BOND-003 trial.
Read More
Phase 3 VERIFY Trial Investigates Rusfertide’s Potential in Polycythemia Vera
July 16th 2024In an interview, Aniket Bankar, MD, discussed the background, design, and goals of the phase 3 VERIFY trial of the hepcidin mimetic rusfertide for the treatment of patients with polycythemia vera.
Read More