Liso-Cel Delivers Deep, Durable Responses in R/R MCL
High complete response rates and low incidences of cytokine release syndrome and neurological events were observed when patients with relapsed or refractory mantle cell lymphoma were treated with lisocabtagene maraleucel.
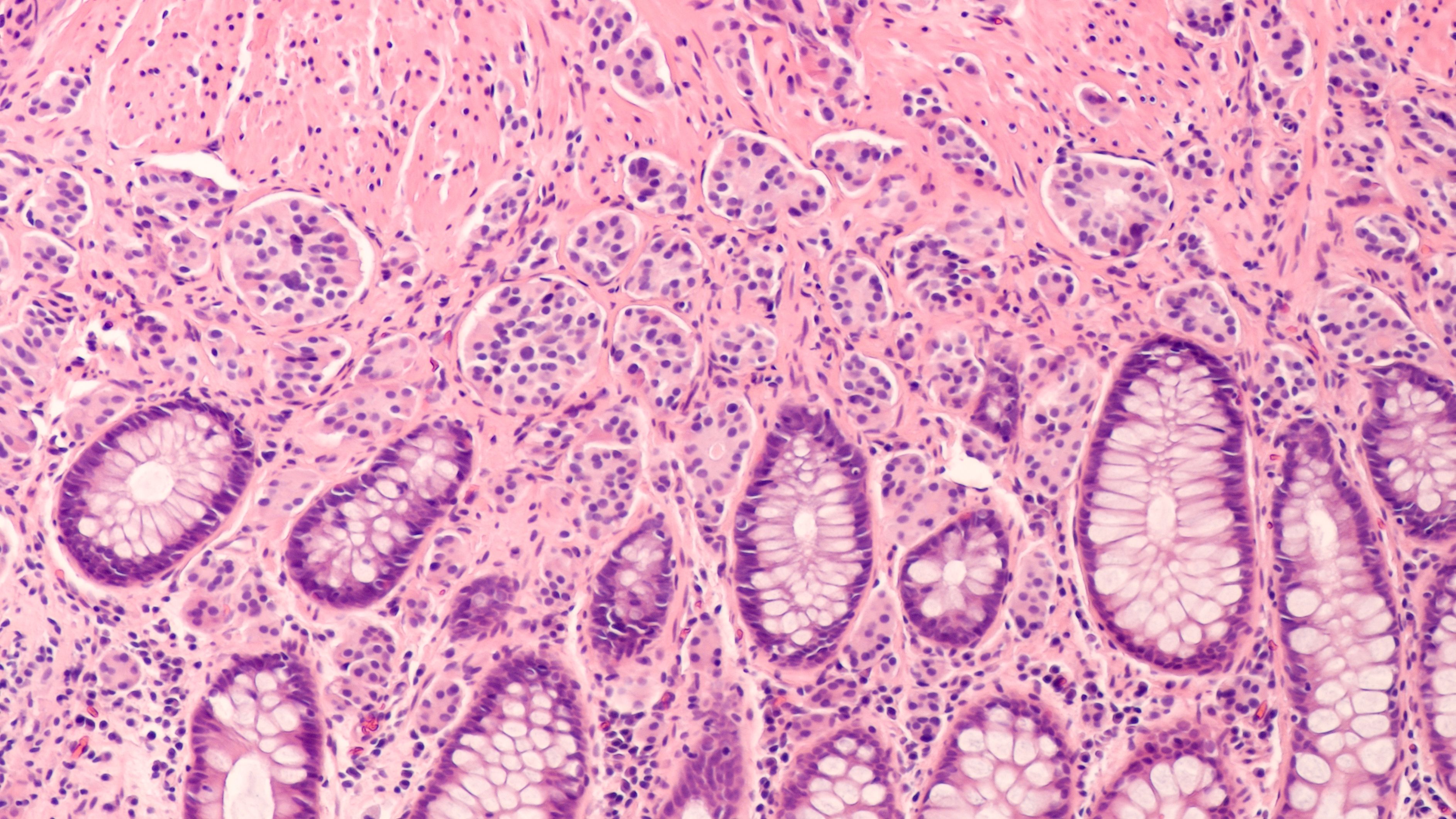
Lymphomas: © David A Litman - stock.adobe.com
The chimeric antigen receptor (CAR) T-cell therapy lisocabtagene maraleucel (liso-cel; Breyanzi) delivered a high complete response (CR) rate and showed a relatively low incidence of grade 3 or higher cytokine release syndrome (CRS) or neurological events (NEs) in patients with heavily pretreated relapsed or refractory (R/R) mantle cell lymphoma (MCL).1
Findings from the MCL cohort of the phase 1 TRANSCEND NHL 001 study (NCT02631044) were published in the Journal of Clinical Oncology. A total of 88 patients who received liso-cel. At a median follow-up of 16.1 months (range, 0.4-60.5), the overall response rate (ORR) was 83.1% (95% CI, 73.3%-90.5%) and the CR rate was 72.3% (95% CI, 61.4%-81.6%). Further, the median duration of response (DOR) was 15.7 months (95% CI, 6.2-24.0), and progression-free survival (PFS) was 15.3 months (95% CI, 6.6-24.9).
CRS was observed in 61% of patients (n = 54), with only 1% of patients (n = 1) experiencing grade 4 CRS and no patients experiencing grade 3 or 5 CRS. NEs were reported in 31% of patients, with 9% of patients experiencing grade 3 or 5 NEs.
“There is an urgent need for CAR T-cell therapy options with low incidence of CRS, NEs, and infections. With a favorable benefit/risk profile and consistent responses in high-risk patient populations (eg, high Ki-67 proliferation index, TP53 mutations, blastoid morphology, and secondary CNS lymphoma), liso-cel may help to address this unmet clinical need,” study authors wrote.
Regarding patient demographics, 73% of patients were aged 65 years and older, and the median age was 68.5 years (range, 36-86). The median number of previous lines of therapy was 3 (range, 1-11). Refractory disease was reported in 69% of patients (n = 61), with 53% of patients (n = 36) refractory to treatment with a Bruton tyrosine kinase (BTK) inhibitor. TP53 mutations were observed in 23% of patients (n = 20), while 31% of patients (n = 27) had blastoid morphology.
The primary end points of the TRANSCEND NHL 001 trial are eaincidence of adverse events (AEs) , probability of dose-limiting toxicities, and ORR. CR rate is the key secondary end point, with other secondary end points including DOR, PFS, overall survival, cellular kinetic parameters, health-related quality of life, and hospitalizations.
Regarding safety, 86% (n = 76) of patients experienced grade ≥ 3 treatment-emergent AEs (TEAEs), andthe most common were neutropenia (56%), anemia (37.5%), and thrombocytopenia (25%). Grade ≥ 3 infections were reported in 15% of patients, while prolonged cytopenia was reported in 25% of patients. Serious TEAEs were observed in 53% (n = 47), and 39% of patients (n = 34) had serious TEAEs that were considered related to liso-cel.
“CAR T-cell therapies continue to evolve in R/R MCL. Both brexucabtagene autoleucel [brexu-cel; Tecartus] and liso-cel target CD19; however, alternative targets are being explored such as BAFF-R and ROR1. Additionally, bispecific antibodies are emerging as a new therapeutic modality, including glofitamab [Columvi}. Studies are still ongoing, and the clinical activity of these therapies has not yet been fully established,” study authors wrote.
“There's nothing that can cure relapsed/refractory MCL outside of CAR T. There's a lot of great drugs out there and I'm very interested in them,” Andre Goy, MD, physician-in-chief, Hackensack Meridian Health Oncology Care Transformation Services, and chairman, chief physician officer, chief, Lymphoma Division, John Theurer Cancer Center, Hackensack University Medical Center, said in an interview with Targeted OncologyTM. “There was a lot of concern in the beginning with CAR T toxicity. We have learned how to manage and are pre-emptive with toxicity. I haven't seen a patient in the [intensive care unit] with CAR T in a long time. Now if we refer patients earlier, they have a 1 and done treatment and we should all go for this.”
REFERENCES:
1. Wang M, Siddiqi T, Gordon LI, et al. Lisocabtagene maraleucel in relapsed/refractory mantle cell lymphoma: primary analysis of the mantle cell lymphoma cohort from TRANSCEND NHL 001, a phase I multicenter seamless design study. J Clin Oncol. Published online December 10, 2023. doi:10.1200/JCO.23.02214
Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen
New APL Treatment Shows Promise: Higher Survival Rates, Less Toxicity
July 6th 2024ATO/ATRA plus idarubicin showed superior 2-year EFS (88% vs 70%) and 5-year EFS (87% vs 55%) compared to ATRA/chemotherapy. The trial indicated lower hematologic toxicity with ATO/ATRA, including reduced rates of thrombocytopenia and neutropenia.
Read More
Different Options Discussed for DLBCL in Later-Lines of Treatment
June 13th 2024During a Case-Based Roundtable® event, Matthew Ulrickson, MD, considered treatments for patients with relapsed/refractory diffuse large B-cell lymphoma with event participants in the second article of a 2-part series.
Read More
Early Data Shows Axi-Cel’s Potential in Treating R/R Primary and Secondary CNS Lymphomas
June 13th 2024Findings from a phase 1 trial presented at ASCO showed that axicabtagene ciloleucel was safe with clinical activity seen among patients with relapsed/refractory primary and secondary central nervous system lymphoma.
Read More