
Henry M. Kuerer, MD, PhD, FACS, professor of surgery, Department of Surgical Oncology, The University of Texas MD Anderson Cancer Center, discusses two ongoing trials that look promising for the treatment of patients with DCIS.

Your AI-Trained Oncology Knowledge Connection!


Henry M. Kuerer, MD, PhD, FACS, professor of surgery, Department of Surgical Oncology, The University of Texas MD Anderson Cancer Center, discusses two ongoing trials that look promising for the treatment of patients with DCIS.

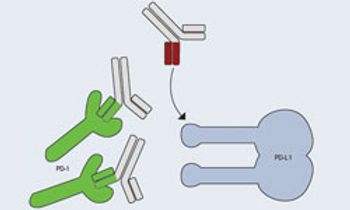
PD-L1 levels adequately predict response and clinical outcomes for PD-1 inhibitor MK-3475 in patients with non-small cell lung cancer (NSCLC) and melanoma.

The large phase III MAGRIT study investigating the MAGE-A3-specific vaccine GSK1572932A for patients with non-small cell lung cancer (NSCLC) will be completely halted following an interim analysis that demonstrated a lack of benefit.
Meir Wetzler, MD, chief, Leukemia Section, Department of Medicine, Professor of Medicine, Department of Medicine, Roswell Park Cancer Institute, discusses a phase I trial that studies the side effects and immune response to DEC-205/NY-ESO-1 fusion protein CDX-1401 and decitabine in patients with myelodysplastic syndrome (MDS) or acute myeloid leukemia

The oncolytic immunotherapeutic vaccine talimogene laherparepvec (T-VEC) promoted tumor shrinkage in 64% of patients with advanced melanoma, including a marked reduction in the size of uninjected metastatic lesions.

Nivolumab, a PD-1-specific antibody, has shown to produce long-term remissions with limited toxicity in patients with advanced melanoma, according to results from one of the longest follow ups to examine the drug.
The MAGE-A3-specific immunotherapeutic GSK1572932A failed to significantly extend disease-free survival (DFS) in patients with resected nonmetastatic non-small cell lung cancer (NSCLC) who tested negative for a specific gene expression signature.

Screening for prostate-specific antigen (PSA) significantly cuts the death rate from prostate cancer, but at the same time, America’s medical community should work harder to avoid the screen’s potential pitfalls.

Robert Figlin, MD, FACP, professor of medicine and biomedical sciences, Steven Spielberg Family Chair in Hematology Oncology, Cedars-Sinai Medical Center, discusses results from a single-arm phase II trial of the autologous dendritic cell immunotherapy AGS-003 plus standard treatment for patients with newly-diagnosed metastatic renal cell carcinoma

Renier J. Brentjens, MD, PhD, associate professor, chief, Cellular Therapeutics Center, Memorial Sloan Kettering Cancer Center, discusses the outlook for CAR-modified T cells.
With the growing knowledge of immune system components, signaling processes, and regulatory networks, cancer immunotherapy has yielded increasingly favorable treatment outcomes.

While the concept of cancer-specific immunotherapy is not new, it recently has been proven feasible as a rational treatment for patients with some of the most challenging and difficult malignancies.

Harriet Kluger, MD, associate professor of medicine (medical oncology), associate director, Hematology/Oncology Fellowship Program, Yale Cancer Center, explains how immunotherapies are changing the treatment of melanoma.

The use of predictive biomarkers in cancer medicine may allow oncologists to target interventions to populations with greater response rates, affect sizes, and benefit-risk ratios.
Work on viruses as antitumor agents began in the 1950s, but advances in molecular biology have provided new tools and new possibilities for engineering their potency, selectivity, and safety.

Balazs Halmos, MD, section chief of Thoracic Oncology at NewYork-Presbyterian Hospital/Columbia University Medical Center, discusses the future of immunotherapy treatments.

Survival rates for patients with cancer have consistently increased in past decades. However, a gap remains in treatment options, particularly for patients with a history of treatment for advanced or recurrent solid-tumor cancers.

A wide-ranging analysis of more than 5500 breast cancer tumors that combined genomic and protein expression testing has identified promising targets to explore for treating patients with poor prognoses, with particularly notable findings involving androgen receptor (AR) expression.

Until recently, the cornerstone of therapy for metastatic melanoma had been chemotherapy with dacarbazine (DTIC) and immunotherapy with high-dose interleukin-2 (HD IL-2) or interferon- (IFN- ).

Antoni Ribas, MD, PhD, professor of medicine, Jonsson Comprehensive Cancer Center, University of California, Los Angeles, discusses the excitement surrounding immunotherapies for the treatment of patients with melanoma.

Naiyer A. Rizvi, MD, an associate attending physician, Memorial Sloan Kettering Cancer Center, discusses PD-L1 as a potential biomarker for immunotherapy agents for patients with lung cancer.

Georgina Long, BSc, PhD, MBBS, FRACP, medical oncologist, translational researcher, Melanoma Institute Australia, The University of Sydney, highlights targeted therapies in development for melanoma.

Renier J. Brentjens, MD, PhD, associate professor, chief, Cellular Therapeutics Center, Memorial Sloan Kettering Cancer Center, discusses the utility of CAR-modified T cells in myeloid malignancies.
There are currently numerous experimental therapeutic options in various phases of clinical development that may hold promise for patients with advanced melanoma.

Harriet Kluger, MD, associate professor of medicine (medical oncology), associate director, Hematology/Oncology Fellowship Program, Yale Cancer Center, discusses the toxicities associated with immunotherapies.